Periodontal disease stages: From mild inflammation to tooth loss
 Periodontal disease is the affection of the tissues surrounding the tooth.
Periodontal disease is the affection of the tissues surrounding the tooth. It is one of the most common diseases in the world and the leading cause of tooth loss in adults.
According to The American Academy of Periodontology, half of the American adults suffer from gum disease. Another study showed that over 90% of the world's population has chronic gingivitis to some degree.
Periodontal disease goes through several stages. Discover them in this article.
What is periodontal disease?
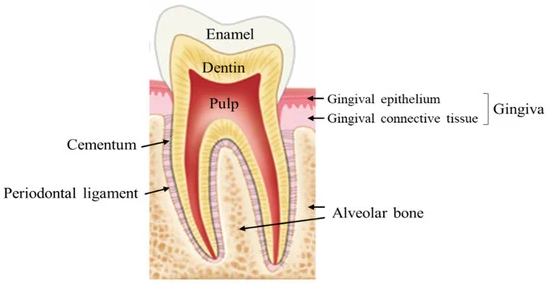 Periodontal disease is an inflammation of the tissues surrounding the tooth, including the bone, ligaments and cementum that cover the root.
Periodontal disease is an inflammation of the tissues surrounding the tooth, including the bone, ligaments and cementum that cover the root.
It involves bacterial plaque and our immune response. Bacteria will invade our gum tissue and trigger inflammation. The molecules released by the bacteria and immune cells will cause tissue destruction.
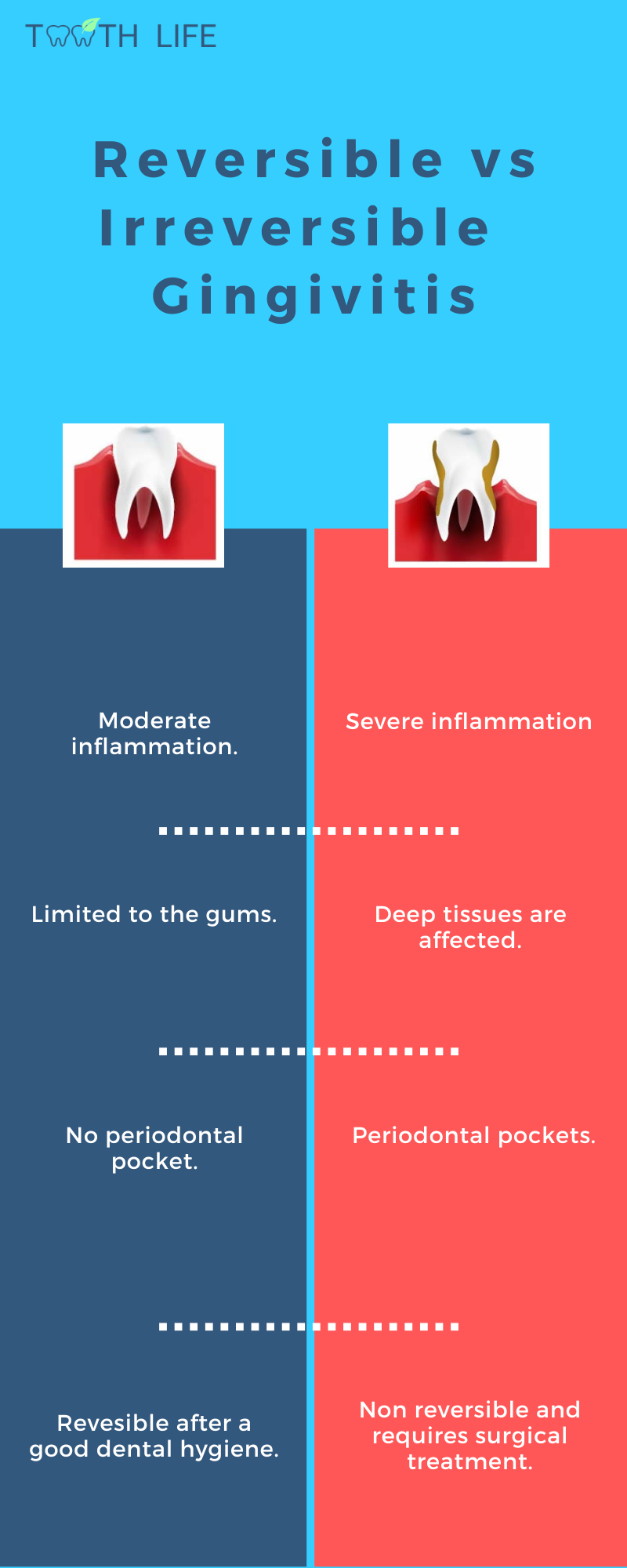
There are two main types of periodontal disease: Gingivitis and periodontitis.
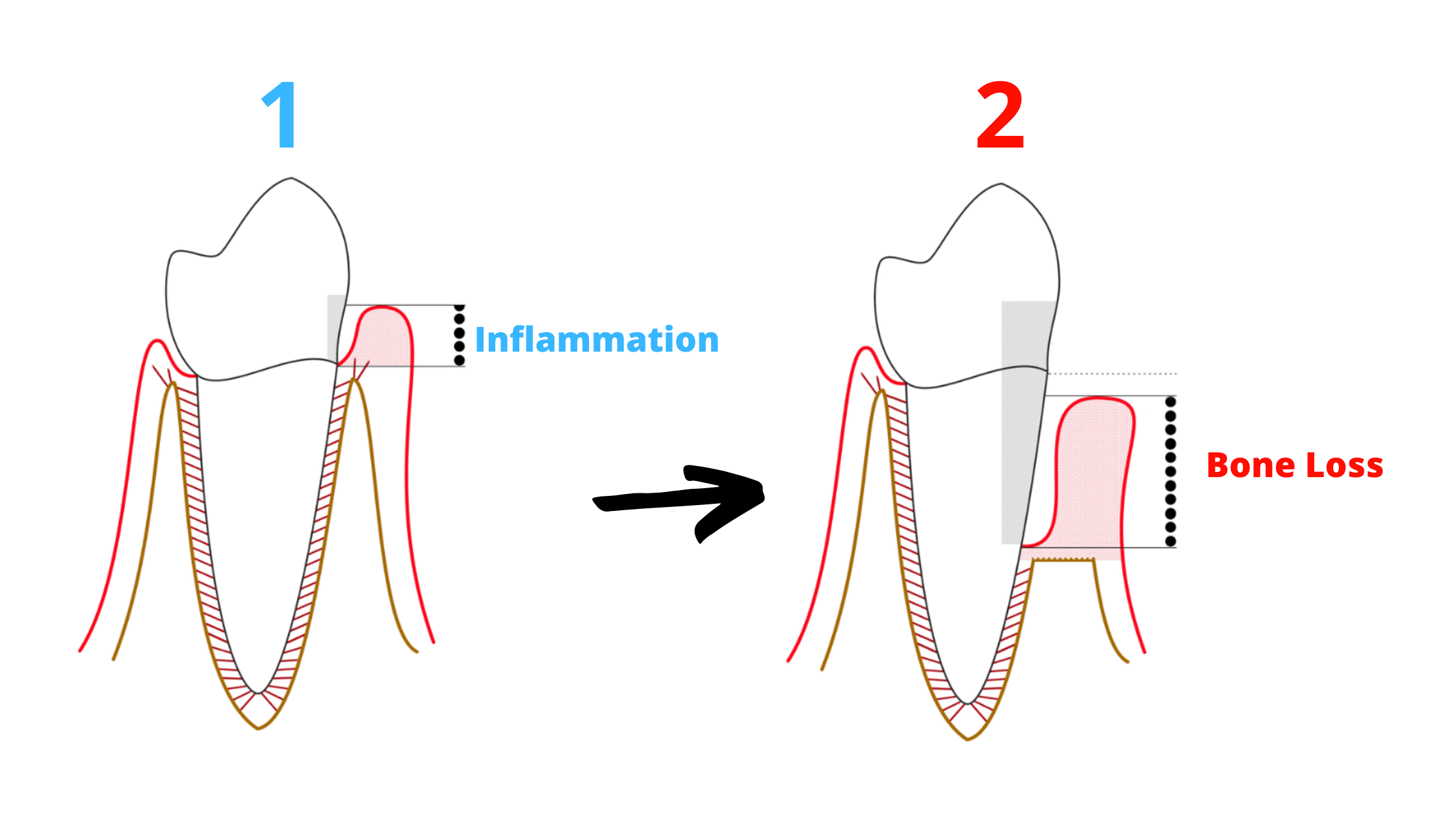
Periodontal disease will first affect the gums, resulting in gingivitis. You will notice changes in your gum such as redness, swelling and bleeding.
Gingivitis is reversible but if left untreated, gingivitis can turn into periodontitis where the deep tissues including the bone and cementum are affected.
In addition to the signs of gingivitis, there is bone destruction which can lead to mobility or even tooth loss.
It is difficult to differentiate between gingivitis and the early stage of periodontitis. The exact diagnosis is confirmed by a clinical and X-ray examination.
Once the bone is affected, the disease is irreversible and requires periodontal treatment by your dentist.
What are the stages of periodontal disease?
Periodontal disease goes through 4 stages. Its progression is different from one person to another. Some people will have rapid bone destruction and will lose all their teeth while others will never lose their teeth.The four stages of periodontal disease are:
Gingivitis
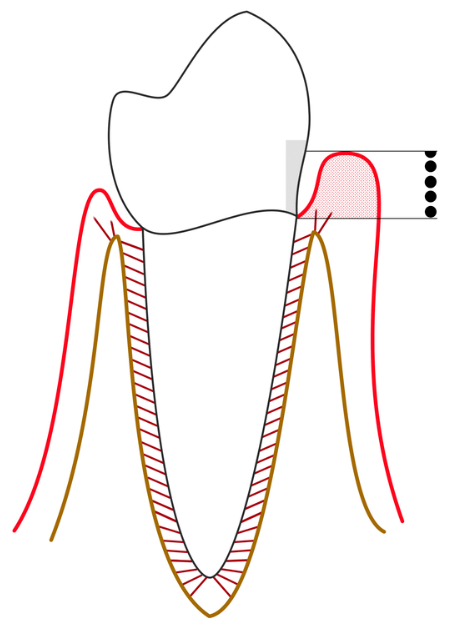
Gingivitis is the earliest stage of periodontal disease.
Mouth Bacteria will accumulate on the teeth and form plaque.
Within the plaque, the bacteria will establish numerous interactions to survive and increase their aggressivity.
The contact of the plaque with the gum will irritate it. An inflammation will then occur.
Signs of gingivitis include:
- Red and swollen gums
- Gums that bleed when you floss or brush your teeth
Gingivitis is reversible but if left untreated, it can turn into irreversible periodontitis.
Early Periodontal Disease
The inflammation has evolved. Swelling and redness of the gums are more visible.The gums tend to bleed randomly and begin to recede.
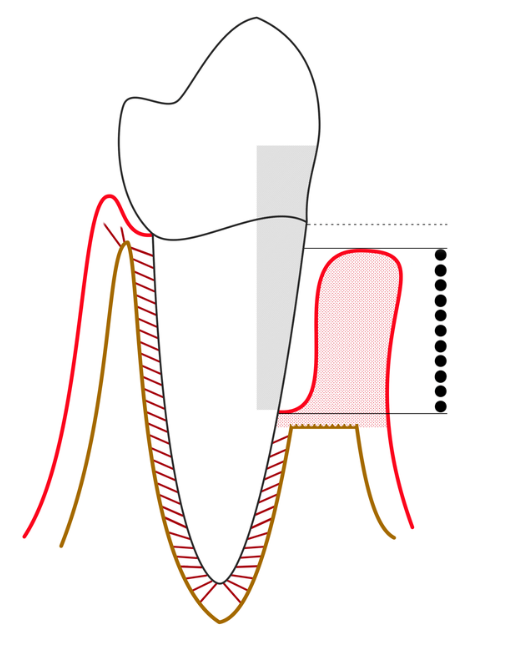
A space between the teeth and the gums called periodontal "pockets" appears.
These pockets provide an ideal environment for bacteria to grow, allowing the inflammation to spread to the bone. The bone that supports the teeth becomes damaged.
This stage is the transition between gingivitis and periodontitis and often goes unnoticed because there is no pain or aesthetic problems.
Moderate Periodontal Disease
The symptoms of periodontitis worsen as the inflammation spreads.
Half of the bone that supports the tooth is destroyed, which causes tooth mobility. You may notice discomfort when eating.
The gums continue to recede and the periodontal pockets will become deeper.
Advanced Periodontal Disease
This is the terminal phase where the tooth will pull away from the bone.
Inflammation has led to advanced tissue destruction.
The tooth is supported only by a small amount of bone. Common signs include:
- Red and swollen gums
- Bleeding gums
- Painful abscess
- Sensitivity to heat
- Loose teeth
- Bad breath or halitosis
- Pain when chewing
Factors that contribute to the progression of periodontal disease

Bacterial plaque
Plaque is a bacterial deposit that sticks to the teeth and can turn into tartar which is more resistant.
The long contact of the plaque with the gum will aggravate the inflammation and lead to periodontitis.
Poor oral hygiene
Poor oral hygiene promotes plaque build-up that can lead to gingivitis.
The plaque must reach a certain amount to trigger periodontal disease. It differ from person to person, some people will never develop periodontitis even if they never brush their teeth.
Age
Age contributes to the increase of plaque build up and decreases the immune defense potential.
Thus, the prevalence and severity of periodontal diseases increase with age, reaching a peak at 60 years old.
Chronic periodontitis is the most common disease in the elderly. It is known by a slow and continuous bone destruction.
Smoking
Smokers are:
- 6 times more likely to develop gum disease
- More periodontal pockets
- More gum recession
- More bone loss.
- More tooth loss.
- Less gum bleeding (which can hide the early signs of gum disease).
Genetic
40-80% of periodontal diseases are genetically inherited. Some people are predisposed to severe periodontal disease, while others are not.
Stress
Stress is an aggravating factor in gum disease. Patients who have difficulty managing stress are at greater risk for severe periodontal disease.
Studies have shown that stress is linked to an increased risk of gum disease. Because when we are stressed, the molecules released by our body depress our immune system and decrease the blood flow of our gums.
Men who report being stressed every day are 43% more likely to develop gum disease than men who report being rarely stressed.
Medical conditions
Certain conditions can aggravate periodontal disease either directly or through medical treatment.
These conditions include diabetes, hemopathies, certain viral infections such as AIDS.
Some medications significantly decrease salivary flow which is bad for our oral health. These include antihypertensives, narcotic analgesics, some tranquilizers, sedatives and antihistamines.
Some medications may be a contributing factor to gum disease. Nifedipine, Cyclosporine and Phenytoin can cause gum swelling.
Other medications, especially those containing added sugar, alter the acidity of the mouth and the composition of dental plaque, making it more likely to adhere to the surfaces of the teeth and promoting the growth of pathogenic bacteria.
How to reverse gingivitis and prevent periodontitis
Plaque is made up of different types of bacteria that establish connections between them to survive and increase their pathogenic factor.You can prevent gingivitis and periodontitis by maintaining oral hygiene. When done consistently, an oral hygiene routine can prevent plaque from building up and causing gum disease.
Prevention will also help to reverse gingivitis and prevent it from turning into periodontitis.
Good oral hygiene habits include:
- Brush your teeth 2 times a day for at least 3 minutes, with a good brushing technique and a soft bristle toothbrush to avoid hurting your gum. Brushing helps remove up to 70% of plaque.
- Floss your teeth once a day. Flossing helps you to eliminate 30% of the remaining plaque between the teeth. You can also use an interdental brush if your teeth are not tight. Oral irrigators can also be effective. A study has shown that oral irrigators may reduce gum inflammation.
- Learn about antibacterial treatments. If you're especially vulnerable to gum disease — for example, because of a medical condition — your dentist may recommend special antibacterial mouth rinses or other treatments to help cut down on harmful bacteria in your mouth.
- Stop smoking. Smoking is a risk factor for gum disease. Quitting smoking will improve your periodontal health.
- Take care of yourself. Some diseases and conditions harm gum health, especially diabetes, some viral infections and hormonal modifications.
