Cracked Tooth After Root Canal? What You Need to Know
 Root canal, also called endodontic therapy, involves treating the inside of the tooth.
Root canal, also called endodontic therapy, involves treating the inside of the tooth.
When the pulp, the soft tissue that carries the nerves and blood vessels, is infected or irreversibly damaged, it must be removed to save the tooth.
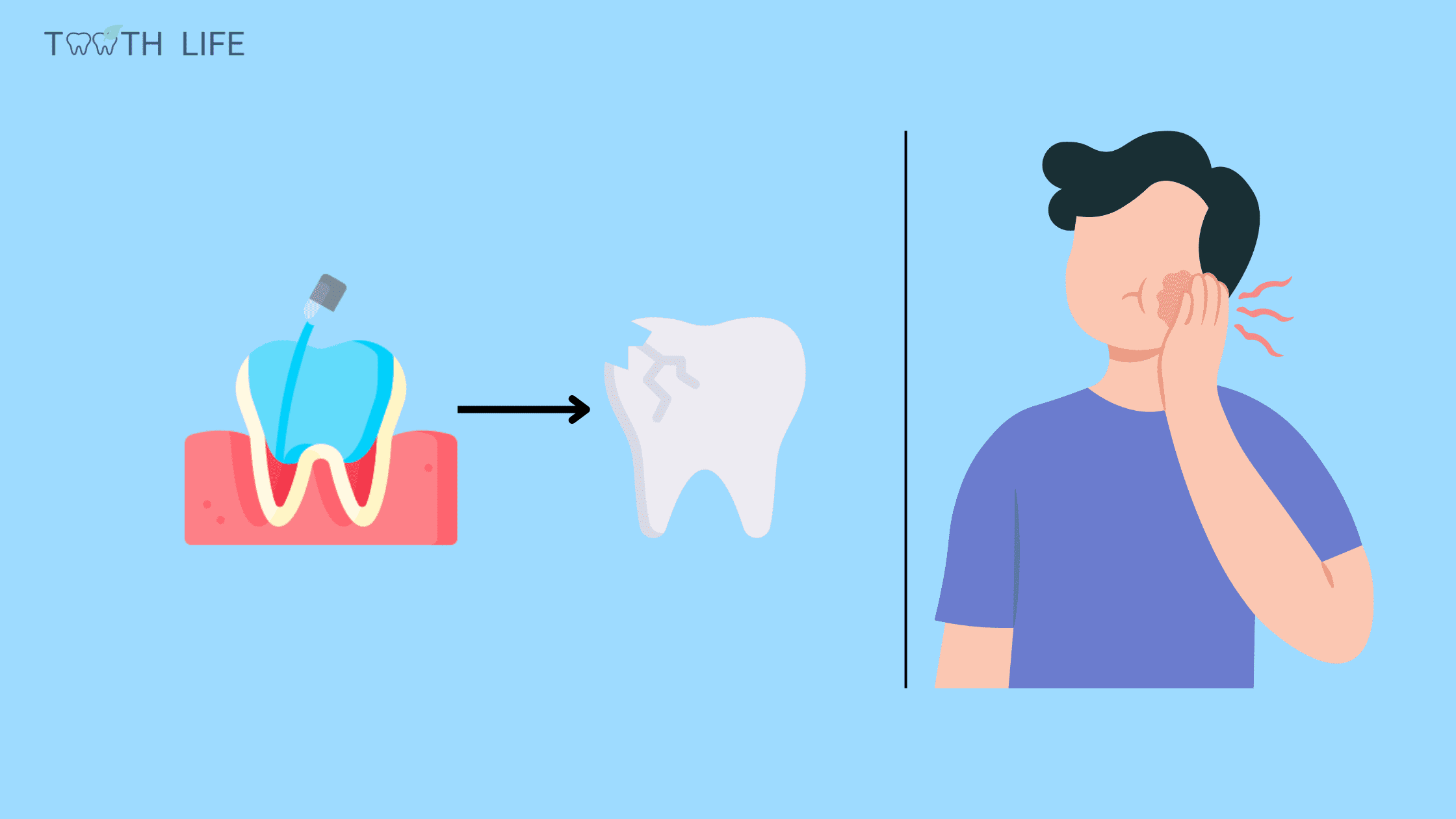
The downside is that although root canal therapy saves the tooth from extraction, it makes it weaker and more prone to fracture. That's why the procedure comes with a dental crown or restoration that will protect the tooth from further damage.
In this article, we will learn why the tooth is more likely to crack after a root canal, the symptoms, and the different treatment options.
1. Why are teeth more likely to break or crack after root canal treatment?
2. Can a cracked tooth after a root canal be saved?
3. How can the dentist diagnose a fracture?
4. How can a fracture occur after a root canal?
5. Complications of a cracked tooth with root canal treatment
Why are teeth more likely to break or crack after root canal treatment?
When a tooth undergoes a root canal, it becomes more vulnerable to fractures compared to a healthy tooth (3). Why? Well, in the process of cleaning, shaping, and filling the root canals, a significant portion of the tooth's support structure is lost. Unless it's shielded by a sound crown, the tooth may easily fracture when subjected to the stress of chewing.
Think of a tooth post-root canal as a dead wood branch—they've both lost their inner vitality, strength, and flexibility. Just as a dead branch can snap under pressure, a tooth that has undergone endodontic treatment is susceptible to breaking due to the absence of its natural internal support system.
The likelihood of a tooth cracking also depends on what led to the need for a root canal in the first place. If the tooth was severely decayed or damaged before treatment, it's already weakened and more prone to breaking.
Moreover, the risk of fracture increases if the tooth has a history of dental work or if it's undergoing a second round of root canal treatment. That's like adding more stress to an already vulnerable structure.
Therefore, it's crucial to consider a solid restoration soon after the procedure to safeguard your tooth from potential injuries that may require its extraction.
Can a cracked tooth after a root canal be saved?
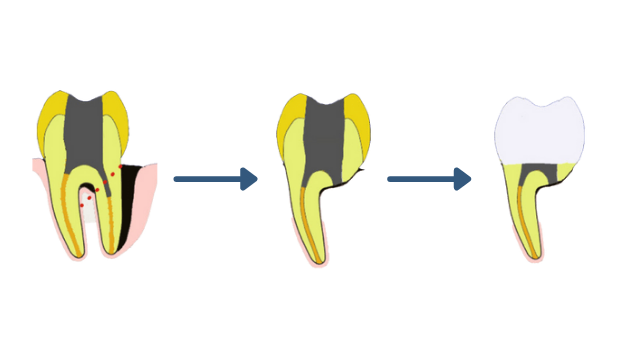
The approach to treating cracked teeth after a root canal depends on the nature, location, and severity of the damage.Usually, when the crack is confined to the crown (the top portion of the tooth), the tooth can still be repaired. Treatment usually involves extracting the loose fragment and capping the tooth with a dental crown.
When the fracture line extends beyond the gum line, there's a risk that bacteria may have seeped into the filling. In this case, the dentist may recommend a new root canal treatment to thoroughly clean the inside of the tooth and prevent the onset of infection.
However, when the injury is severe, penetrating deep into the roots, preserving the tooth becomes challenging. If the tooth cannot adequately support a proper restoration, removal may be the necessary course of action.
So, how to effectively address a weakened tooth that has undergone a root canal? The answer lies in prevention. The most secure approach is to restore the tooth as soon as possible. Additionally, here are some tips to prevent complications that may lead to treatment failure:
- Prioritize Dental Hygiene: Ensure optimal oral health by gently brushing your teeth at least twice a day with a soft-bristled toothbrush, daily flossing, and regular dental check-ups every six months. This routine helps prevent cavities and infections that can further weaken the tooth.
- Protect Against Teeth Grinding: If you grind your teeth at night or engage in contact sports, consider investing in a mouthguard.
- Steer clear of biting or chewing on hard objects: Chewing on hard objects, such as ice cubes, is too damaging for the tooth. Getting rid of these habits will minimize the strain and increase your tooth longevity.
How can the dentist diagnose a fracture?
A cracked tooth may be visible or felt by your tongue if the fracture line is thick enough. However, it can be hard to spot in its early stages. You may notice it until it becomes symptomatic, leading to pain or a gum abscess. To diagnose the fracture, your dentist will:- Do a visual test: They will look for the fracture line to assess its extent and direction on the tooth.
- Expose the tooth to light: Your dentist may expose your tooth to a light source to reveal any injury.
- Remove the restoration: They may remove the restoration (filling or crown) to directly assess what is happening inside the tooth.
- Use an endodontic microscope: To better visualize cracks.
- Perform a periodontal probing: Using an instrument, they will evaluate the tissues surrounding the tooth to assess the extent of the fracture on the roots.
- Surgery: Only performed if a root fracture is suspected and cannot be revealed by other methods. The gum is cut and peeled away from the tooth to allow a direct view of the root.
- Take an X-ray: 3D digital radiography allows a three-dimensional assessment of the cracked tooth. It is the best and least traumatic tool for the diagnosis of dental fractures.
How can a fracture occur after a root canal?
After a root canal treatment, various types of fractures can manifest. These fractures may be confined to the crown, presenting as a fractured cusp or cracked tooth syndrome, or extend to the root, resulting in vertical root fractures.The way these injuries initiate and progress also vary. They can occur spontaneously, especially if the tooth was already compromised, or progress gradually as a result of external factors such as excessive pressure (biting a hard object) or habits such as grinding or clenching the teeth.
1. Vertical root fracture:

This is the most common type of fracture after root canal treatment. The injury starts from the root and progresses towards the crown. It mainly results from the treatment itself, which can make the roots more brittle.
Vertical root fractures are often associated with complications in the gum tissue, such as infections and abscesses.
Treatment:
Extraction is often the go-to solution, particularly for teeth with one root (front teeth). In fact, vertical root fracture is the third most common reason for pulling out a tooth with a root canal (2).
For molars with multiple roots, there's a potential way to save the tooth. It involves removing the damaged part and keeping the healthy portion in procedures known as root resection and tooth hemisection.
Root Resection (1)
2. Fractured cusp:

A fractured cusp is the easiest to reveal. It is a fracture that starts at the crown and ends at or slightly below the gum line. It is often the result of a tooth weakened by severe decay, a large filling or excessive biting forces.
Treatment:
Fractured cusp is the least devastating and can often be repaired. If the fracture line does not extend beyond the gum line, your dentist will start by removing the loose fragment and capping your tooth with a crown.
However, if the damage extends into the roots, a crown lengthening procedure may be necessary before restoration.
3. Cracked tooth syndrome:
The fracture typically begins at the crown and moves towards the roots, mainly affecting the back teeth like molars and premolars. Without treatment, it can advance, potentially splitting the tooth in half.
Treatment:
If the fracture line is limited to the crown, the tooth can be restored and saved. However, if the fracture extends beyond the gum line and deep into the roots, extraction may be the only option.
4. Split tooth:

This type of fracture divides the tooth into two halves, often as a result of an untreated injury. Symptoms may include loosening of the tooth, pain or discomfort when chewing, and, sometimes, the appearance of a gum boil or abscess.
Complications of a cracked tooth with root canal treatment
A cracked tooth following a root canal might not cause any noticeable symptoms initially—it can be asymptomatic for a while.However, if left unattended, the crack can irritate the gums and result in an infection of the tissues around the tooth. Symptoms may vary from mild discomfort to intense pain, especially while eating.
In severe situations, an abscess may develop near the affected tooth, accompanied by symptoms like redness, swelling, and the discharge of pus.
- Endodontic Diagnosis Pathology and Treatment Planning Mastering Clinical Practice by Bobby Patel
- Vertical root fractures and their management https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4001262/
- Systematic review fracture resistance of endodontically treated posterior teeth restored with fiber reinforced composites- a systematic review
- An interdisciplinary approach to treat crown-root-fractured tooth https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821233/
- An innovative approach for treating vertically fractured mandibular molar - hemisection with socket preservation https://www.jidonline.com/article.asp?issn=2229-5194;year=2012;volume=2;issue=2;spage=141;epage=143;aulast=Agrawal
- Novel Matricing Technique for Management of Fractured Cusp Conundrum – A Clinician’s Corner https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4866268/
