Gingivitis vs. Periodontitis
The mouth is one of the most bacteria-rich parts of the body. Under healthy conditions, oral bacteria maintain the right balance without causing any harm. But when they grow and proliferate, they form plaque and tartar, which irritates the tissues and leads to gum disease.There are two main types of gum disease: gingivitis and periodontitis. In this article we will learn about the differences between them.
What is gingivitis?
According to The American Academy Of Periodontology, half of the American adults suffer from gum disease. Another study showed that over 90% of the world's population has chronic gingivitis to some degree.Gingivitis is an inflammation of the gums. It is the early stage of gum disease when the damage is still reversible.
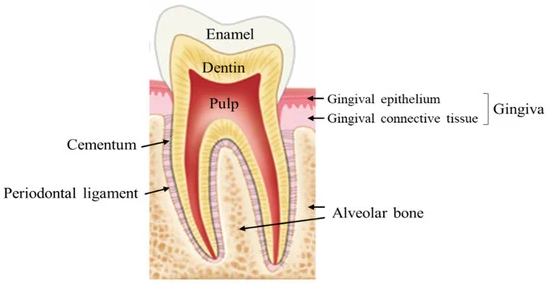
At this stage, the inflammation is limited to the gums and has not yet reached the deep tissues that attach the tooth to the bone.
The gums will appear red and swollen and may bleed when brushing or chewing. Gums that tend to bleed on their own indicate a severe form of gingivitis.
If left untreated, gingivitis can progress to periodontitis, where the damage is irreversible.
What is periodontitis?
 Periodontitis is also an inflammatory disease. However, the damage has now spread to the deeper tissues.
Periodontitis is also an inflammatory disease. However, the damage has now spread to the deeper tissues.
In periodontitis, the inflammation has reached the tissues that hold the tooth in place. These include the bone, the ligaments, and the cementum that covers the root.
Periodontitis leads to periodontal pockets, which are enlarged spaces between the teeth and gums. They are filled with bacteria, toxins, and debris and are inaccessible to brushing and regular cleaning. The only way to reach and clean these areas is with a professional deep cleaning at your dentist's office, also known as scaling and root planing.
Symptoms of periodontitis include:
- Red and swollen gums
- Bleeding gums
- Tender teeth
- Sore gums
- Bad breath
- Tooth mobility
- Increased space between teeth (Diastema)
- Pain during chewing
- Receding gums
How can gingivitis turn into periodontitis?
Under normal conditions, oral bacteria live in harmony with our immune system.When the balance is disturbed for various reasons (poor oral hygiene, smoking, and some medical conditions), harmful bacteria dominate and overgrow.
Bacteria accumulate in plaque, a soft, sticky, whitish deposit. When plaque hardens, it turns into tartar, which is more difficult to remove.
Plaque and tartar irritate the gums and cause local inflammation, resulting in gingivitis. The gums then become red, swollen and tend to bleed.
If left untreated, the inflammation can progress deeper and irreversibly damage the deep supporting tissues of the tooth.
Gradually, the gums pull away from the teeth, causing them to recede. At the same time, the bone resorbs and the teeth become loose. In extreme cases, the teeth may even come out.
From gingivitis to periodontitis: The risk factors

Different factors can cause gingivitis to turn into periodontitis. These include:
Bacterial plaque
Plaque is a bacterial deposit that sticks to the teeth and can turn into tartar which is more resistant.
The long contact of the plaque with the gum will aggravate the inflammation and lead to periodontitis.
Stress
Stress is an aggravating factor in gum disease. Patients who have difficulty coping with stress are at greater risk of severe periodontal disease.
Many studies have shown this link. Men who report being stressed every day are 43% more likely to develop gum disease than those who are not.
Smoking
Smokers are:
- 6 times more likely to develop gum disease
- More periodontal pockets
- More gum recession
- More bone loss.
- More tooth loss.
- Less gum bleeding (which can hide the early signs of gum disease).
Infections
Certain infections, such as the human immunodeficiency virus (HIV), can increase the risk of gum disease by weakening our immune system.
Studies have shown that HIV-infected populations have more bone loss and gum recession than non-HIV populations.
Certain drugs
Some medications significantly reduce salivary flow, which is bad for oral health. These include antihypertensives, narcotics, some tranquilizers, and sedatives.
There are also others that are known to increase gum swelling. These include nifedipine, cyclosporine, and phenytoin.
Other medications, especially those with added sugar, increase mouth acidity and disturbs the microbial balance, promoting the growth of pathogenic bacteria.
Prevention
Plaque contains different types of bacteria that work in synergy to survive and increase their aggressiveness.You can prevent gingivitis and periodontitis by practicing good oral hygiene. This will help prevent the build-up of plaque and tartar, the primary causes of gum disease. Among the best practices to adopt at home:
- Brush your teeth 2 times a day for at least 3 minutes, with a good brushing technique and a soft bristle toothbrush to avoid hurting your gum. Brushing helps remove up to 70% of plaque.
- Floss your teeth once a day. Flossing helps you to eliminate 30% of the remaining plaque between the teeth. You can also use an interdental brush if your teeth are not tight. Oral irrigator can also be effective. A study has shown that oral irrigator may reduce gum inflammation.
- Learn about antibacterial treatments. If you're especially vulnerable to gum disease — for example, because of a medical condition — your dentist may recommend special antibacterial mouth rinses or other treatments to help cut down on harmful bacteria in your mouth.
- Stop smoking. Smoking is a risk factor for gum disease. Quitting smoking will improve your periodontal health.
- Take care of yourself. Some diseases and conditions harm gum health, especially diabetes, some viral infections and hormonal modifications.
