Periodontal bone grafting: The regenerative approach
 Periodontal disease can have a devastating impact, leading to the loss of bone around your teeth and affecting your smile and overall well-being. Thankfully, regenerative methods like bone grafting offer a solution to rebuild your bone and extend the life of your teeth.
Periodontal disease can have a devastating impact, leading to the loss of bone around your teeth and affecting your smile and overall well-being. Thankfully, regenerative methods like bone grafting offer a solution to rebuild your bone and extend the life of your teeth.
In this article, you will learn about when a bone graft is necessary, the various periodontal bone grafting techniques, the pros and cons of each approach, alternative treatments, the healing process, and essential aftercare.
1. How can periodontal disease cause bone loss?
2. When do you need a bone graft surgery to treat gum disease?
3. The different types and techniques of periodontal bone grafting:
4. Are there other alternatives to bone grafting?
5. What can I expect after the bone graft?
6. What are the healing stages of a bone graft?
7. Aftercare:
How can periodontal disease cause bone loss?

Periodontal disease is a common reason why people lose their teeth. It happens when plaque, a sticky layer of bacteria, builds up on your teeth and causes inflammation. At first, it affects your gums and makes them red, swollen, and bleed easily. This is called gingivitis. If you don't treat it, it can get worse and become periodontitis.
Periodontitis is when the inflammation spreads to the tissues that hold your teeth in place. This includes the ligaments and the bone. The bacteria can damage these tissues, making your teeth loose and eventually fall out.
When it comes to treating periodontal disease, there are two main approaches.
The first is non-surgical periodontal therapy, which involves addressing the root cause of the disease. This typically includes a deep cleaning procedure called scaling and root planing, as well as improving your oral hygiene habits at home.
The second is surgical periodontal therapy, which tries to repair deeply damaged tissues. This may involve different methods, such as regenerative surgery, which can use grafts to fill in the bone defects.
However, you must know that surgery is only a complementary treatment of the first phase. Not everyone needs it.
So, if the non-surgical therapy successfully heals your gum tissues and stops the progression of the disease, you may not need surgery at all. (1)
When do you need a bone graft surgery to treat gum disease?
Periodontal bone grafting is a regenerative surgery that aims to restore the damaged bone around teeth. It can help prevent tooth loss and improve the appearance and function of your teeth.However, not everyone with gum disease needs a bone graft. Before considering this option, you need to complete the first phase of treatment, which involves non-surgical methods (oral hygiene, scaling and root planing, antibiotics, etc.)
This phase can often reverse some of the bone loss and reduce the inflammation and infection in your gums.
You also need to address any risk factors that may worsen your condition, such as smoking, diabetes, or tartar accumulation.
Only after completing this phase and assessing the results can your periodontist determine if you need a bone graft or not.
A bone graft may be recommended if you still have deep pockets or bone defects around your teeth that make them unstable or prone to infection.
By filling these defects with bone or bone-like materials, your periodontist can stimulate new bone growth and enhance the support and health of your teeth.
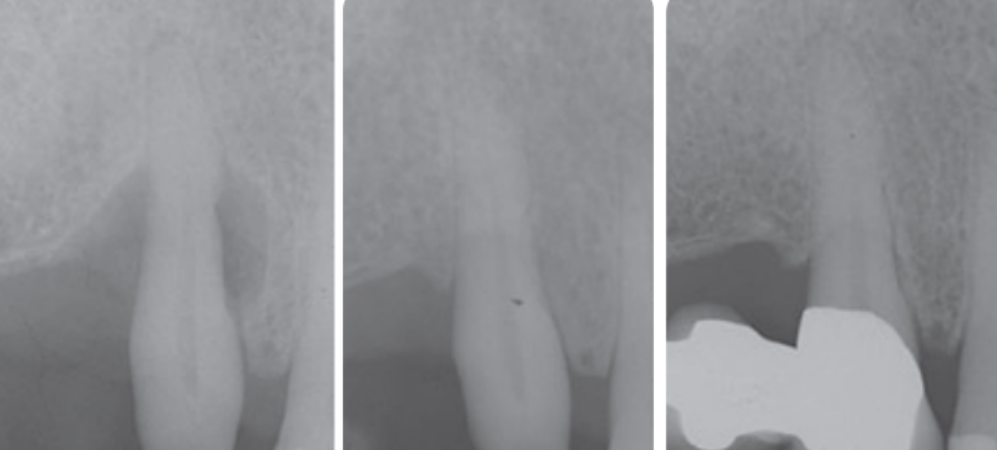
Periodontal bone graft before and after
Factors influencing the outcome of bone grafting:
- Periodontal disease control: You need to treat and prevent the infection that caused the bone loss in the first place. Otherwise, the bone graft may fail or become infected.
- Smoking status: Smoking can harm the healing process and reduce the success rate of bone grafting. If you smoke, you should quit or reduce smoking before and after treatment. Research has shown that smokers tend to have less tissue attachment than non-smokers after surgery. (6)
- Oral hygiene habits: You need to keep your mouth clean and healthy to support the healing and regeneration of the bone. This means brushing, flossing, and visiting your dentist regularly for check-ups and cleanings.
- Bone defect characteristics: The shape, size, and location of the bone defect can affect the outcome of the grafting procedure. Your dentist may use different techniques or materials depending on the type of defect you have.
- General health conditions: Some medical conditions, such as diabetes, can interfere with the healing and success of bone grafting. You should inform your dentist of any health issues you have and follow their instructions carefully.
The different types and techniques of periodontal bone grafting:
There are various types and techniques of periodontal bone grafting, all aimed at filling the defects with bone or synthetic materials to promote healing and regeneration.
Autogenous bone graft: This type of graft uses your own bone as the donor material. The bone can be harvested from your mouth (such as the chin or the back of the jaw) or another area of your body (such as the hip or the shin).
Autogenous bone grafts are considered the gold standard in periodontal bone grafting, as they provide live bone cells and growth factors that can stimulate new bone formation and integration with the surrounding tissues.
Allograft: This type of graft uses human bone from a cadaver as the donor material. The bone is processed and sterilized to remove any potential contaminants and diseases.
Xenograft: This type of graft uses animal bone, typically from cows or pigs, as the donor material. The bone is processed to remove any organic components, leaving behind a mineral matrix that can support new bone growth.
Alloplast: This type of graft uses synthetic materials, such as ceramics or calcium-based compounds, as the donor material. These materials mimic the structure and composition of natural bone and provide support for new bone formation.
Pros & Cons of autogenous bone graft:
Are there other alternatives to bone grafting for gum disease?
Some interesting techniques allow for tissue regeneration without the need for bone grafts. The idea is to create the right environment for cells to rebuild the damaged tissue. Some of these alternatives include:- Guided tissue regeneration: This technique involves using a barrier membrane to separate the gum tissue from the bone defect. The goal is to prevent fast-growing gum tissue from invading the slower-healing bone area. This provides time for the bone and periodontal ligament cells to regenerate.
- Enamel matrix proteins (Emdogain): These proteins help stimulate the regeneration of all tissues that hold the tooth, including bone, cementum, and periodontal ligament. The good part is that enamel matrix proteins are naturally found on a developing tooth. This means we are using something that the body knows well.
- Growth factors: These are substances that naturally occur in the body and play a crucial role in tissue healing and regeneration. By applying specific growth factors to the affected areas, it is possible to stimulate the cells involved in bone and tissue regeneration, enhancing the healing process.
- Platelet Rich Plasma (PRP): PRP is a concentration of platelets obtained from your own blood. Platelets contain growth factors that can accelerate tissue healing and regeneration.
What can I expect after the bone graft?
After the bone grafting procedure, you can expect some post-operative effects. Swelling, pain, and a little bit of bleeding are common. These symptoms usually peak on the third day after the surgery and then subside gradually over the next week.In the first week, the gum will quickly return to its normal appearance. Sutures can usually be removed after 7-10 days. However, bone healing can take longer, up to several months, as it is a gradual and complex process.
What are the healing stages of a bone graft?
In general, here are the stages the bone graft goes through during the healing process:- Inflammatory response: This stage lasts for a few days and constitutes your body's natural reaction to the graft. It helps prepare the site for healing.
- Vascularization: During this stage, which lasts for a few weeks, new blood vessels grow into the graft. This provides oxygen and nutrients to the healing cells.
- Resorption: Your body begins to break down and absorb the graft material. This stage lasts for several months and releases factors that stimulate new bone formation.
- Remodeling: This final stage involves the new bone becoming stronger and integrating with your existing bone, resulting in a stable and healthy bone structure.
However, it's important to note that the healing process and duration can vary depending on different factors. These include the size and type of the graft, your overall health condition, and how well you follow the post-operative care instructions.
Aftercare:
Here are some tips that can help you ensure a quick and optimal recovery:- Prevent bleeding: After the procedure, you must keep the dressing in the surgical site for a few minutes. If bleeding occurs later, apply clean gauze to the site with gentle pressure for 15 minutes.
- Don't rinse, spit, or touch the wound for the first 24 hours: The first day is when the blood clot forms, which is crucial for the healing process. It's important to avoid disturbing or destabilizing the blood clot, as it could result in bleeding and delay the healing.
- Medication: Take any prescribed medications, such as pain relievers or antibiotics, as directed by your periodontist.
- Applying cold: Use an ice pack or a cold compress wrapped in a thin cloth and apply it gently to the outside of your cheek near the surgical area. This can help reduce swelling and provide temporary pain relief. Repeat this process several times throughout the first 24 hours, 10 to 15 minutes at a time.
- Stick to soft foods: Choose soft, easy-to-chew foods that won't irritate or dislodge the surgical site. Opt for nutritious options like soups, yogurt, smoothies, and mashed vegetables. Avoid hot and spicy foods that can cause discomfort.
- Gentle oral hygiene: Maintain good oral hygiene by brushing your teeth gently and avoiding the surgical site for the first week. Use a soft-bristled toothbrush and be cautious around the area to prevent discomfort or disruption of the healing process.
- Saltwater rinse: From the second day on, mix warm water with a teaspoon of salt and gently rinse your mouth several times a day, especially after meals. This can help keep the surgical site clean and reduce the risk of infection.
- Antibacterial mouthwash: Use an antibacterial mouthwash as prescribed by your dentist or periodontist. This can help reduce the bacterial load in your mouth and promote healing.
- Avoid smoking and alcohol: Smoking and alcohol consumption can delay healing and increase the risk of complications. It is best to avoid these habits during the recovery period.
- Avoid strenuous activities: Take it easy for a few days and avoid activities that may increase blood pressure or strain the surgical site. Physical exertion can lead to increased pain and swelling.
- Phase 2 Therapy Periodontal Surgery—Corrective Phase https://pocketdentistry.com/phase-2-therapy-periodontal-surgery-corrective-phase/
- How to Select Replacement Grafts for Various Periodontal and Implant Indications - Hsu - 2013 - Clinical Advances in Periodontics - Wiley Online Library
- Autogenous cortical bone and bioactive glass grafting for treatment of intraosseous periodontal defects - PMC (nih.gov)
- F2105012227.pdf (iosrjournals.org)
- F2105012227.pdf (iosrjournals.org)
- Effect of cigarette smoking on periodontal healing following GTR in infrabony defects. A preliminary retrospective study https://pubmed.ncbi.nlm.nih.gov/7790529/
- Biological principles of bone graft healing https://www.sciencedirect.com/science/article/abs/pii/S1067251696800615
- La cicatrisation des greffes osseusesBone graft healing https://www.sciencedirect.com/science/article/abs/pii/S0035176805858371

