My Actual Risk of Nerve Damage After Wisdom Teeth Removal
Wisdom teeth removal can be challenging, but recovery is usually smooth, and complications afterward are rare. However, in some cases, a nearby nerve may be damaged during the procedure. Although usually minor and temporary, the deficit can sometimes be long-lasting and permanent.
In this article, we'll look at the potential risks, symptoms to be aware of, causes, and treatment options for nerve damage following wisdom teeth removal.
In this article, we'll look at the potential risks, symptoms to be aware of, causes, and treatment options for nerve damage following wisdom teeth removal.
In this article:
1. How likely are you to have nerve damage during wisdom tooth removal?
2. What Nerves are More Likely to be Affected?
3. What increases the risk of nerve damage?
4. What type of nerve damage can occur in wisdom tooth extraction?
5. I feel a tingling sensation after anesthesia. Is this normal?
6. What are the most common symptoms?
7. Can nerve damage lead to facial paralysis?
8. When does recovery from nerve damage usually occur?
9. Nerve damage treatment
10. Should wisdom teeth that carry a risk be left in place?
How likely are you to have nerve damage during wisdom tooth removal?
So, what exactly is nerve injury or damage? During a wisdom tooth removal, there is a rare but potential risk where a crucial nerve may be damaged or, in extreme cases, severed. This can result in various disturbances of sensations, often described as numbness, tingling, or itching in certain areas of the face and mouth.The symptoms you may experience can refer to different conditions, including Paresthesia (sensitivity disturbances), Dysesthesia (burning sensations and pain), or Anesthesia (total loss of sensation). The severity of these symptoms depends mainly on the extent of the injury and the specific nerve affected during the procedure.
Now, back to our question: How likely are you to experience nerve damage during wisdom tooth removal? The risk varies based on several factors, including the position and location of your tooth, whether it's impacted, its proximity to nerves, and your age.
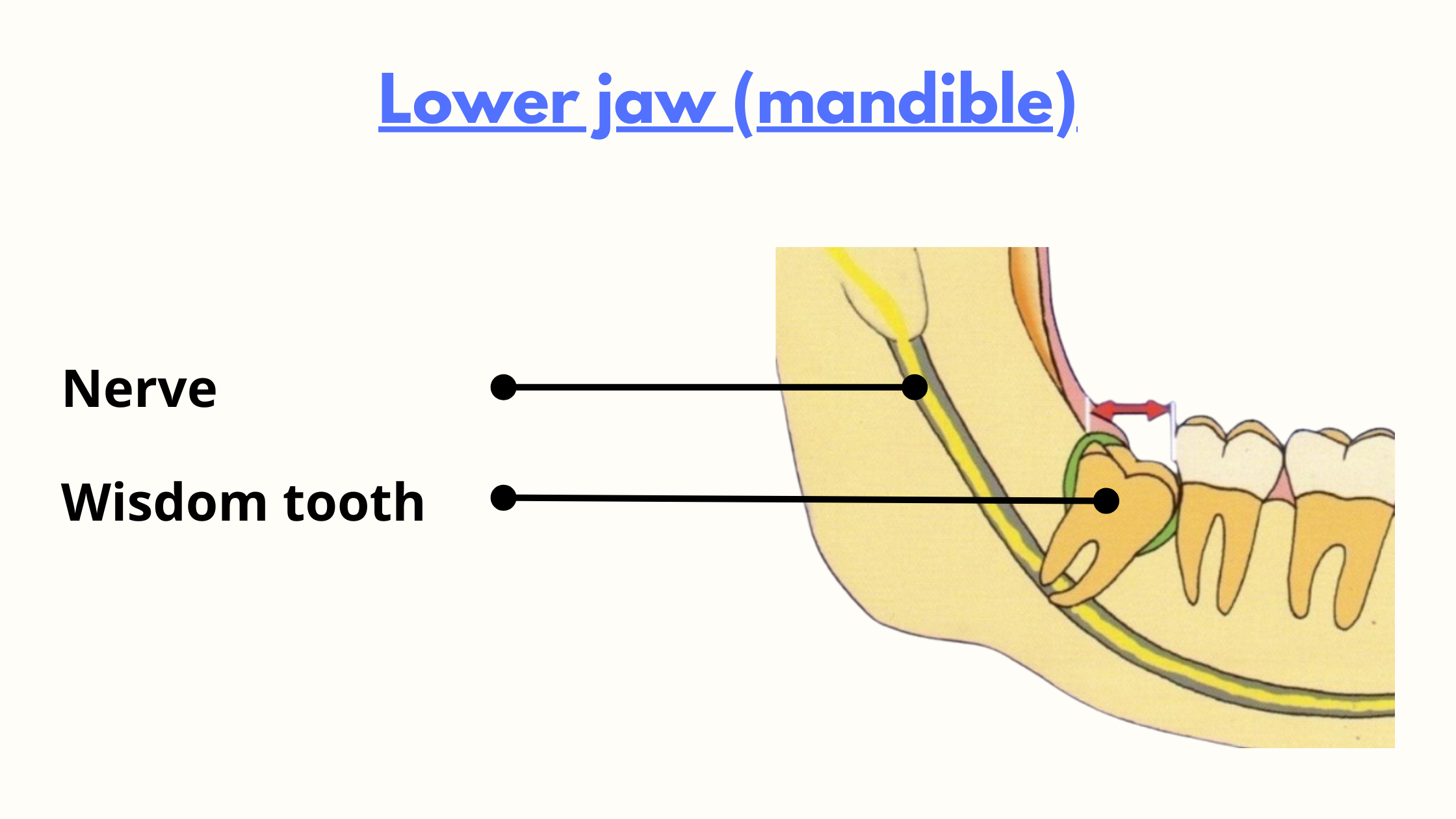
Additionally, the type of tooth being extracted also matters, with lower wisdom teeth carrying a higher risk due to their close relationship with the major nerves of the lower jaw.
The good news is that the overall risk is relatively low, ranging between 0.35% to 8.4%, according to many studies (1,2).
Even if it does happen, most cases are temporary and typically resolve themselves after a few weeks or months.
Permanent sensory disturbances are exceptionally rare, accounting for no more than 2% of cases (1).
What Nerves are More Likely to be Affected?
The nerves most likely affected during wisdom tooth removal are the inferior alveolar nerve (also called the mandibular nerve) and the lingual nerve. Both branch off from the trigeminal nerve, which controls facial and mouth sensibility.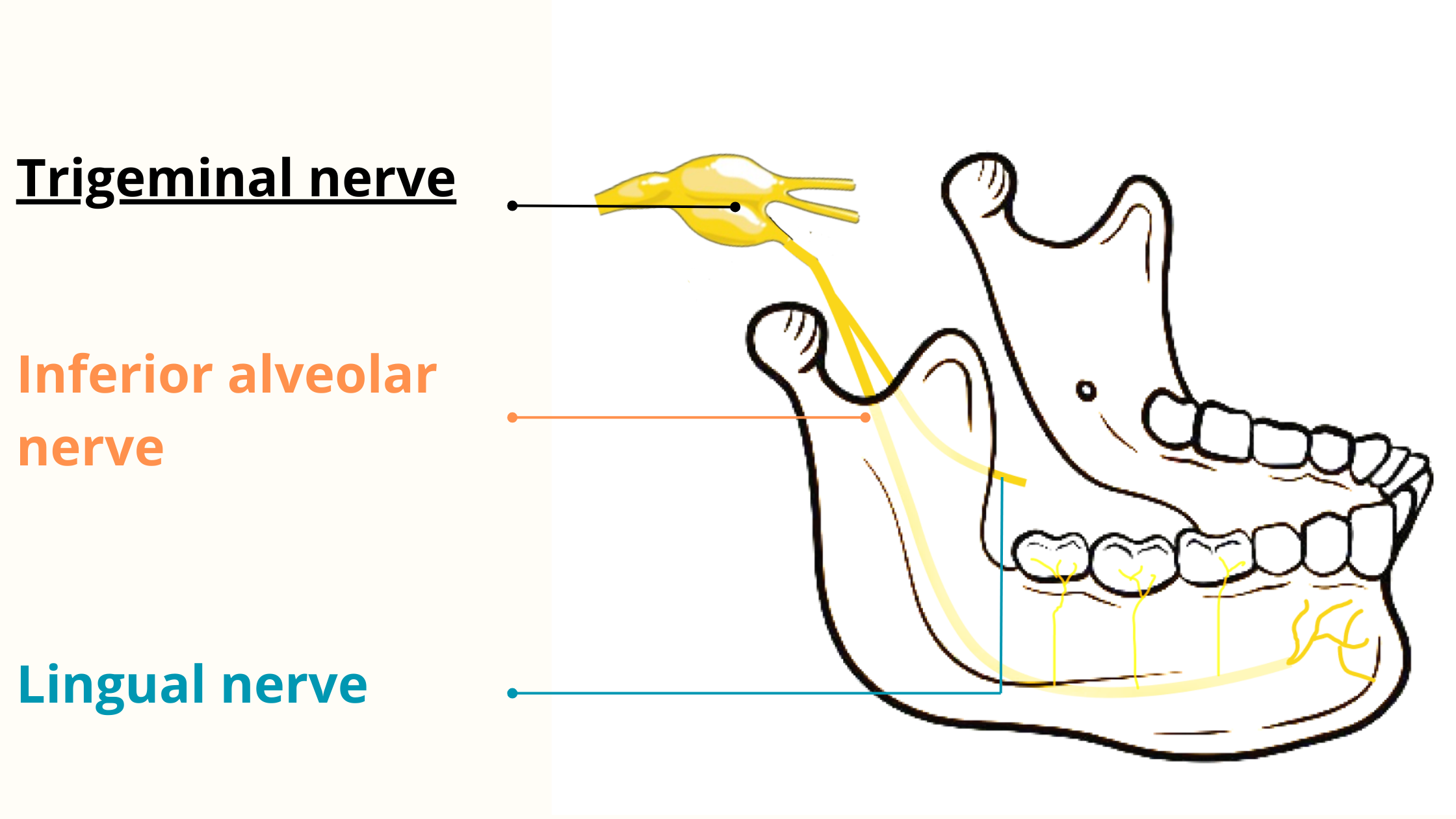
These nerves travel down to the lower jaw, passing near the wisdom teeth. In some instances, they may even be in direct contact with the tooth, increasing the likelihood of injury.
Another important thing to note is that both the lingual and mandibular nerves are sensory, meaning they transmit sensations like temperature, touch, and pain to the brain. They do not control facial muscle movements.
Therefore, when these nerves sustain damage, you may experience sensitivity issues, but by no means paralysis or loss of control over your facial expressions.
What happens when the lingual nerve is damaged?
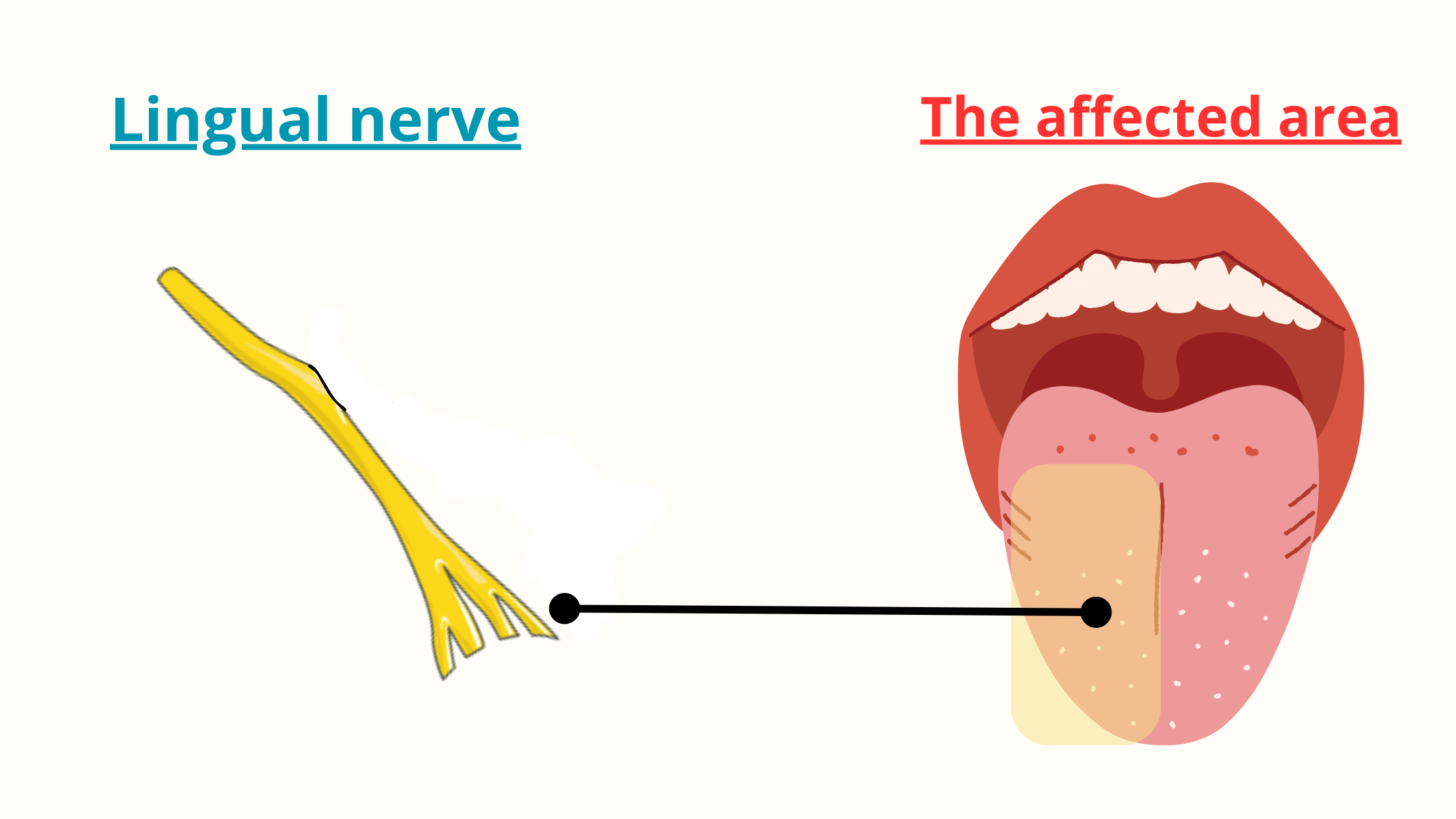
The lingual nerve is responsible for the sensitivity of a significant portion of the tongue (front two-thirds), the floor of the mouth (area under the tongue), and the gums on the inner side. Damage to this nerve can lead to loss of sensitivity in the tongue, affecting your sense of taste and other associated areas. Additionally, as the lingual nerve is involved in the innervation of salivary glands, you may experience reduced saliva production and dry mouth.
Effects of inferior alveolar nerve damage
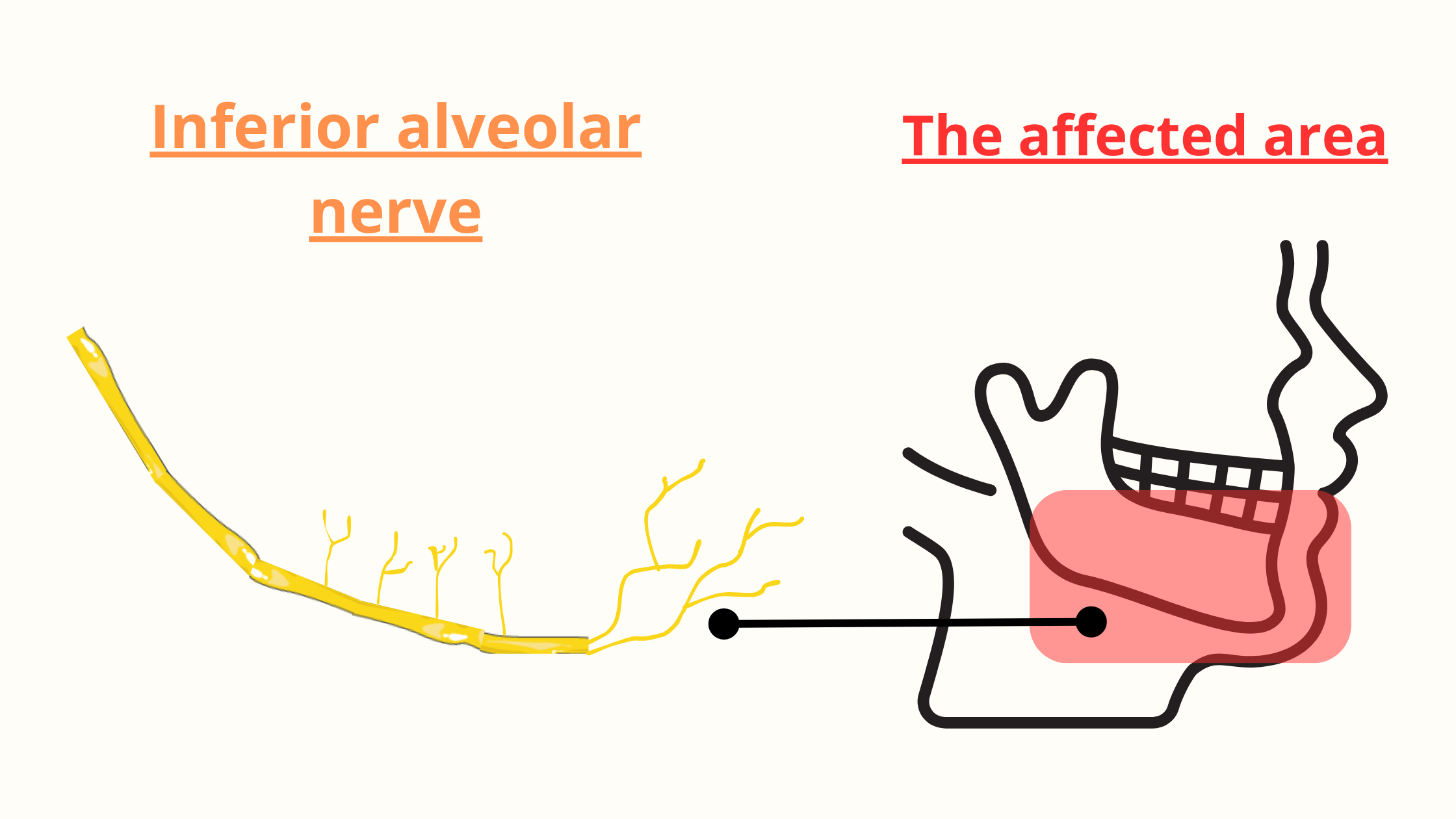
On the other hand, the inferior alveolar nerve provides sensation to the teeth, the front part of the gums, the lower lip, and the chin. Injury to this nerve can result in numbness in all these areas.
What increases the risk of nerve damage?
The risk of damaging a nerve during wisdom tooth removal depends primarily on its proximity to the tooth. In cases where the nerve lies far from the tooth, the risk is practically non-existent.However, when the nerve runs very close to the tooth—whether on its front or back sides or even between the roots—there is a heightened risk of damage during the extraction procedure.
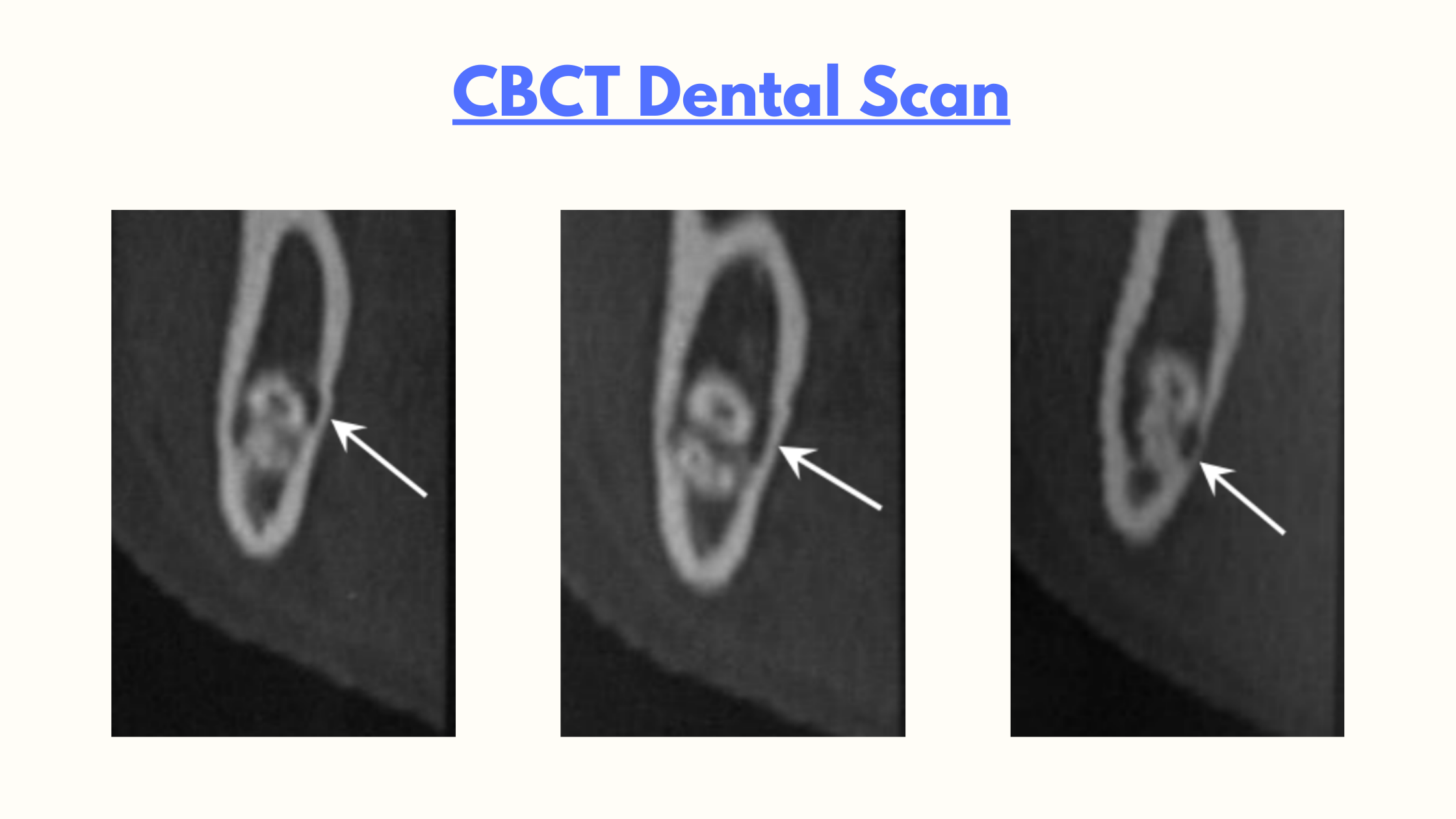
To effectively assess this risk, we often use two radiographic tools: Panoramic X-ray and the CBCT scan.
When the nerve is too close to the tooth, it may appear on a Panoramic X-ray as a deviated or discontinuous trajectory or a darkening of the roots, indicating overlapping.
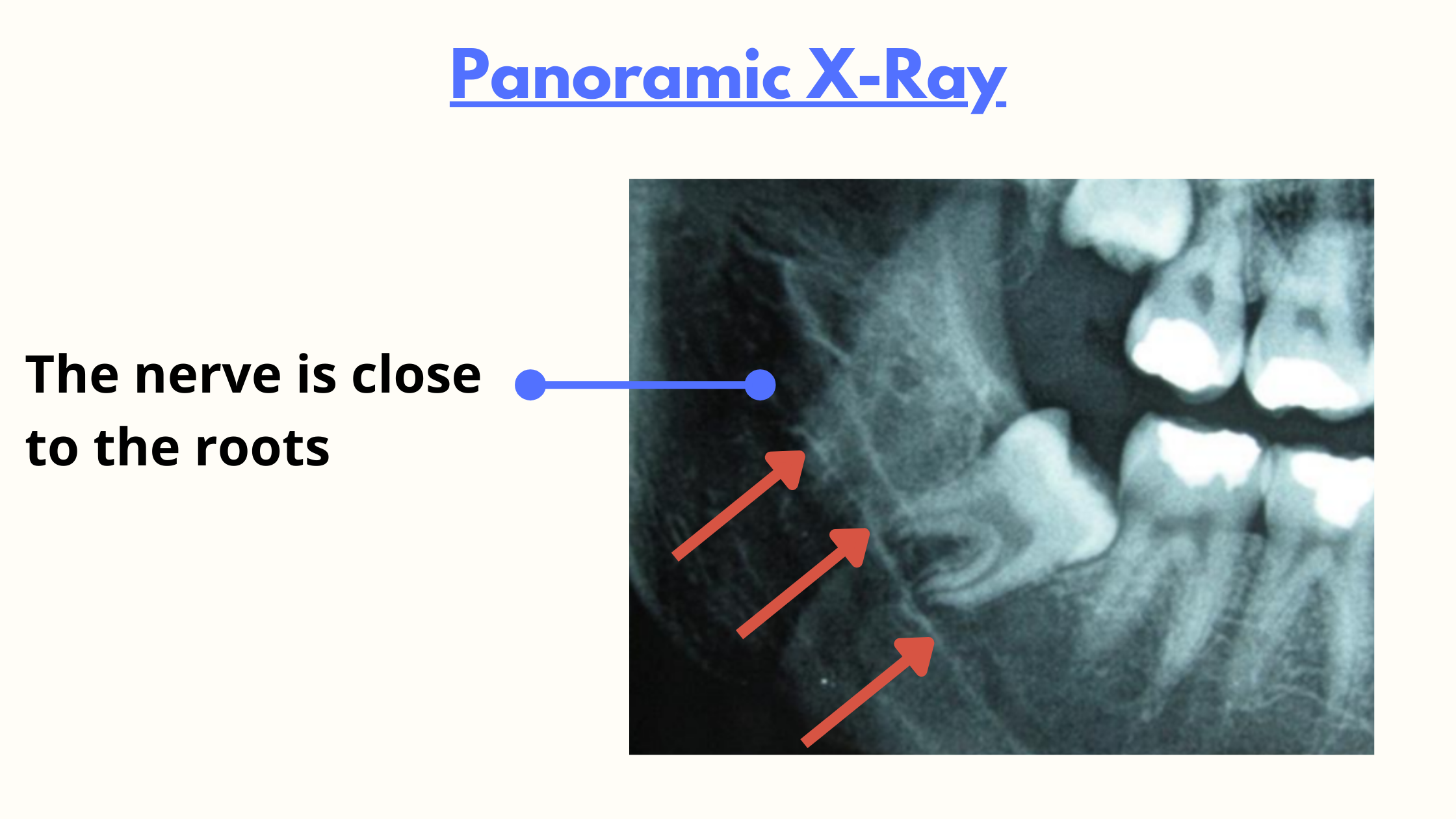
In cases where panoramic doesn't provide detailed information, we turn to the CBCT scan, which offers a more accurate three-dimensional view.
Age is another significant factor influencing the risk of nerve injury during wisdom tooth removal. Between the ages of 18 and 20, wisdom teeth are shorter and still forming. The surrounding bone is softer and more flexible, making extraction at this stage generally easier with fewer complications.
After the age of 30, wisdom teeth are fully developed. While the procedure can still be straightforward if the tooth has fully emerged, removing impacted teeth can be more challenging and carry higher risks.
What type of nerve damage can occur in wisdom tooth extraction?
Nerve injury can be classified by its cause:
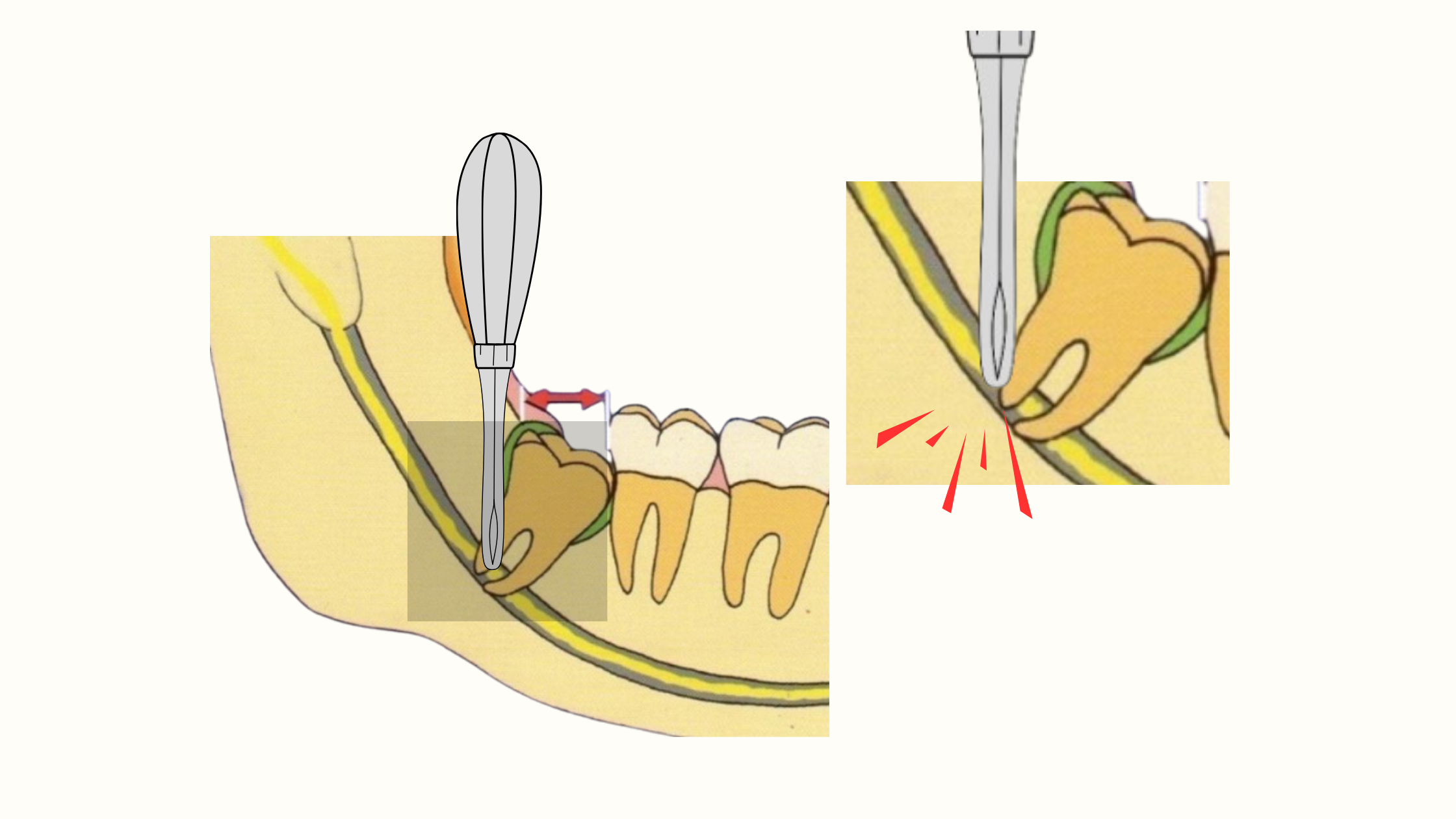
- The accidental contact of the nerve with a sharp instrument used during the extraction. The injury may be a simple irritation or, in extreme cases, a cut.
- The injury happened during the administration of anesthesia. The needle used for the injection may pierce a nerve, causing lasting nerve complications.
- Indirect irritation due to the post-operative swelling and bruising. Post-operative edema can exert pressure on and compress the nerve, leading to strange sensations. Typically, these sensations subside rapidly as the swelling diminishes.
Nerve damage can be distinguished based on its severity:
In most cases, the injury is a simple stretching or rubbing of the nerve, causing temporary sensory disturbances that rapidly resolve as the nerve regenerates.
In more severe instances, the nerve may be completely cut, leading to more pronounced symptoms and the possibility of permanent loss of sensation in the affected area.
However, even when the deficit seems permanent, sometimes recovery can still occur months or years later.
Occasionally, sensations may arise suddenly weeks after the procedure, known as delayed paresthesia. But like other forms of irritation, it is temporary and resolves as the healing process progresses.
I feel a tingling sensation after anesthesia. Is this normal?
Feeling a tingling sensation in your lower jaw right after anesthesia injection is a positive sign that the anesthesia is taking effect. This sensation should resolve within a few hours after the procedure.On the other hand, if the nerve is damaged by the needle, lasting complications may arise. These persist even after the anesthetic has worn off.
In rare cases, if the needle is inserted too deeply, it can damage the facial nerve that controls facial expression. This can result in temporary facial paralysis, which should resolve within a few hours.
What are the most common symptoms?
After the procedure, swelling and some discomfort are a normal part of the recovery process. These should gradually improve over time.However, the only way to tell for sure that it's a nerve injury is to monitor the symptoms and see if they persist for longer than expected.
It's important to note that even if symptoms persist for an extended period, recovery is most likely during the first 6 months, and potential improvement continues for up to 24 months.
The symptoms of nerve damage can vary in intensity, ranging from mild to severe. Here are the most common signs to be aware of:
Sensation impairment:
This may manifest as tingling and itching sensations on the lower lip, lower cheek, chin, and tongue.
Intense, radiating pain:
Some individuals may experience intense, radiating pain, often described as a burning sensation. This pain may extend to other parts of the face and can occur periodically, lasting for hours.
Complete loss of sensation:
In cases where the nerve is completely severed, there may be total numbness in the innervated territory, indicating a more severe form of nerve damage.
Disturbance of oral functions:
Nerve damage can lead to difficulties in oral functions, such as speaking, and an increased tendency to accidentally bite the lip or tongue.
Taste impairment and dry mouth:
The lingual nerve, which passes near the lower wisdom tooth, carries nerve fibers that control taste and saliva production. Damage to these nerves can result in problems like dry mouth, bad breath, and loss of taste, impacting oral health.
Can nerve damage lead to facial paralysis?
Again, nerve damage near wisdom teeth is primarily sensory and does not control facial movements. Therefore, an injury at this level cannot lead to paralysis.After the wisdom tooth removal procedure, it's not uncommon to experience difficulty opening your mouth, speaking, or chewing. These reactions are typically normal. Swelling, bruising, and the surgical process itself can impact the muscles of the jaw, temporarily impeding their proper function.
Additionally, the prolonged mouth opening during the procedure may affect the joints and overall jaw function.
These reactions are temporary and should gradually diminish over time. However, if these difficulties persist, don't hesitate to talk to your dentist.
When does recovery from nerve damage usually occur?
Nerves possess a remarkable ability to regenerate, and recovery typically takes place within the first six months post-surgery. If symptoms persist beyond this timeframe without showing signs of improvement, there is a possibility that the damage may become permanent. However, it's important to note that recovery can continue for up to 24 months in some cases.Nerve damage treatment
If your dentist has confirmed nerve damage your nerve has been damaged or severed, there's no need to panic. Several treatment options are available to address this issue.The primary approach is to allow time for natural healing, particularly for minor and temporary problems. This is particularly true for the inferior alveolar nerve, which may take longer to heal.
In cases where symptoms persist or are severe, a surgical procedure may be considered. This intervention aims to decompress and repair the damaged nerve, restoring its function and sensation. The procedure may involve bringing the severed nerve ends together to facilitate regeneration and the consolidation of both ends.
Should wisdom teeth that carry a risk be left in place?
Deciding whether to remove or keep your wisdom teeth depends on considering the risks and benefits. Your dentist will help you make the best choice by discussing the potential outcomes of the procedure with you.If your wisdom teeth have erupted correctly and contribute positively to your chewing function, extracting them may not be necessary.
However, when these teeth lack sufficient space to position themselves correctly, they can lead to various problems, such as infections, cavities, cysts, and pain. In such cases, the benefits of extraction often outweigh the procedure risks.
But what if a wisdom tooth must absolutely be removed but is too close to a nerve? In such situations, a thorough radiographic examination is crucial to prevent potential nerve complications.
If X-rays have shown that the nerve goes into the roots and that an injury is unavoidable, a technique to bypass this risk is called coronectomy. It involves removing only the crown of the tooth while leaving the roots in place.
Nevertheless, this technique has its limitations, particularly in cases of infection, tumors, or when the tooth is positioned horizontally.
- Delayed paresthesia of inferior alveolar nerve after dental surgery: case report and related pathophysiology - PMC (nih.gov)
- Inferior Alveolar Nerve Injury after Mandibular Third Molar Extraction: a Literature Review - PMC (nih.gov)
- Inferior Alveolar Nerve Deficits and Recovery Following Surgical Removal of Impacted Mandibular Third Molars - PMC (nih.gov)
- Management and prevention of third molar surgery-related trigeminal nerve injury: time for a rethink - PMC (nih.gov)
- Lingual Nerve Injury: Surgical Anatomy and Management (oralhealthgroup.com)

