Bone Loss After Tooth Extraction: Rates, Risks, and Consequences
Losing some bone after tooth extraction is natural and unavoidable, but there are ways to minimize it. If neglected, it may progress to substantial jawbone loss.
In this article, we'll explore the progression rate of bone loss after extraction, the associated risk factors, the consequences, and the diverse options for treatment and prevention.
In this article, we'll explore the progression rate of bone loss after extraction, the associated risk factors, the consequences, and the diverse options for treatment and prevention.
In this article:
1. What Exactly Does It Mean When a Piece of Bone Comes Off During Tooth Extraction?
2. Is Bone Damage Common During Tooth Extraction, and Should I be Concerned?
3. What may Cause the Bone to Come Out During the Extraction Procedure?
4. How Can the Dentist Manage the Situation?
5. What are the possible complications?
Bone Loss After Tooth Extraction is an Unavoidable Process
After a tooth extraction, losing some bone is expected. This happens naturally during healing and continues afterward.During their lifetime, teeth stimulate the bone where they lie (called the alveolar bone) by transmitting the forces exerted during chewing. This activates blood flow and bone cells, enabling the bone to retain its shape and structure.
However, when teeth are missing, the alveolar bone loses its stimulation. The body perceives it as redundant and unnecessary, prompting a process of gradual removal called resoption. In essence, the body likes to save energy by breaking down what it deems useless.
While this energy-saving mechanism benefits the body, it poses challenges for us. Lack of bone can lead to various dental issues and complicates replacement procedures, such as implants.
The Rate of Bone Loss After Tooth Extraction
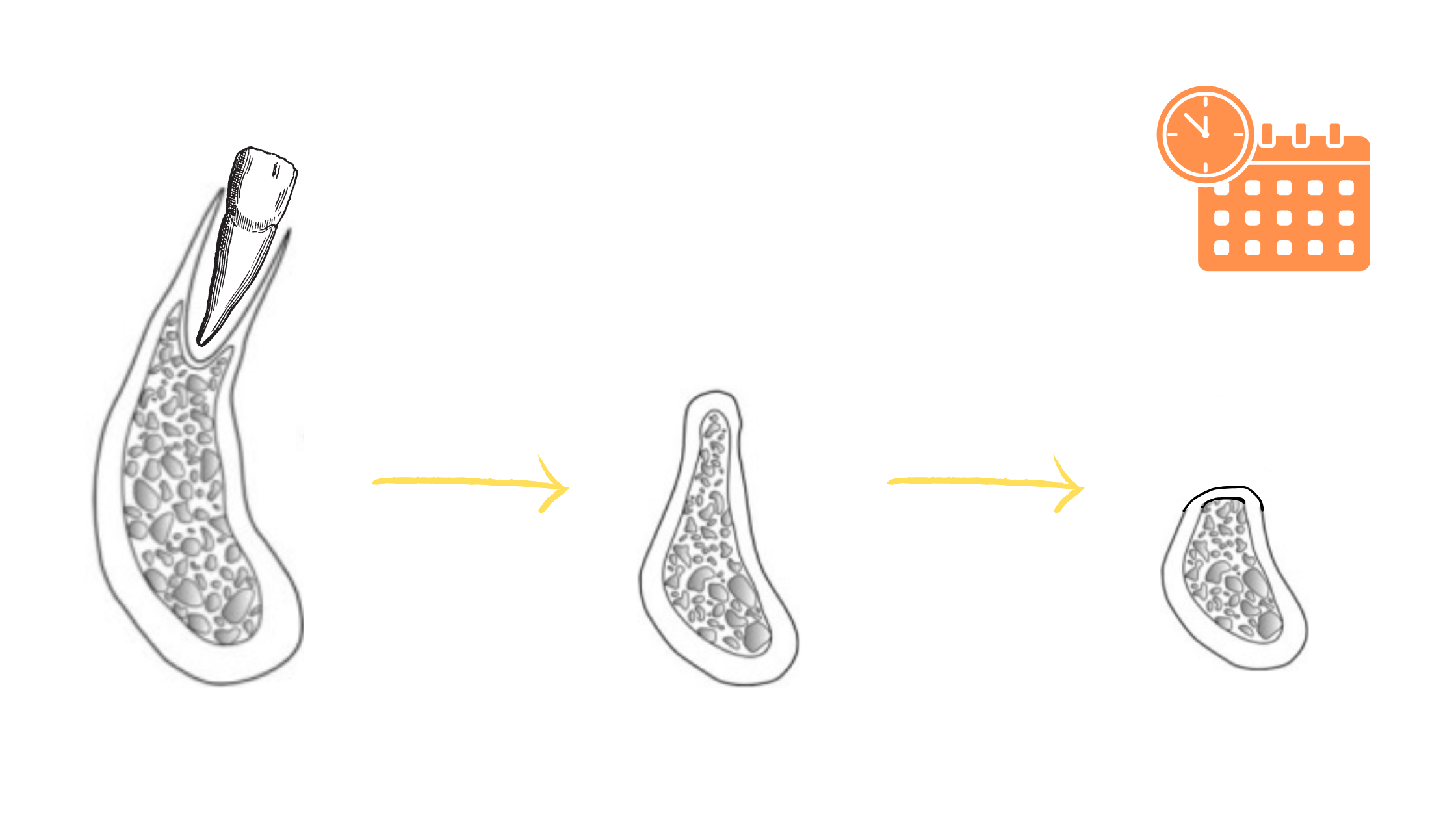
After tooth extraction, the bone loses volume at a much more rapid rate in the initial months.In the first six months,the height of the bone reduces by 11-22%. The width decreases rapidly by 32% at 3 months and 29-63% at 6-7 months.
On average, this means losing about 4mm in thickness and 1mm in height over the initial six months.
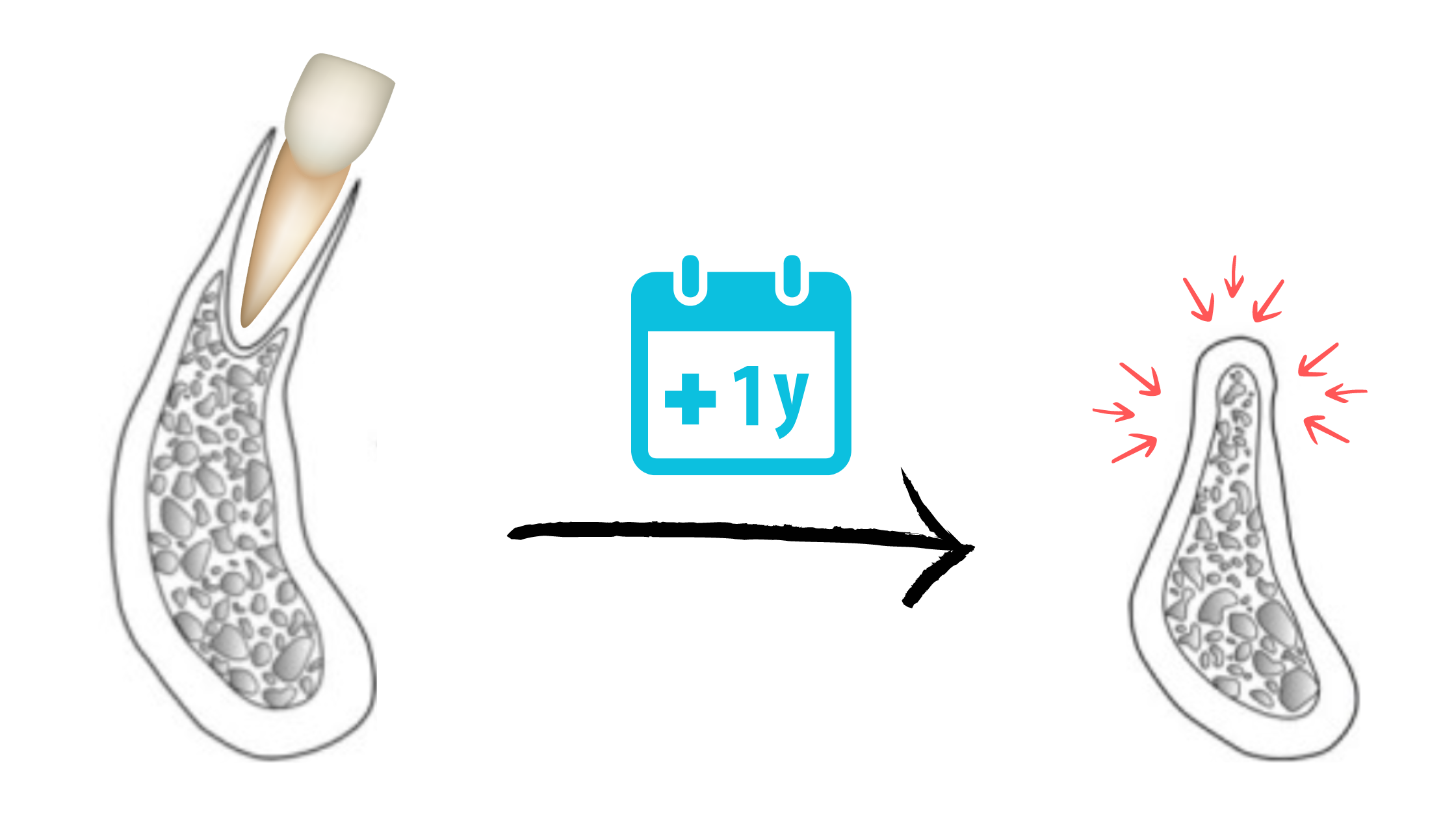
After the first year, approximately 50% of the bone may be lost, and then the resorption process continues at a slower pace, approximately 1% per year.
After two and a half years, bone loss may reach up to 80%, at which point it can stop and stabilize. However, if factors like poor oral hygiene, smoking, certain medical conditions, and specific medications are present, it may continue to progress and worsen.
Risk Factors
Factors such as oral hygiene, nutrition, overall health, medications, and age can impact the rate of bone loss. Typically, after the age of 50, the breakdown of bone (resorption) tends to exceed bone formation, leading to an acceleration in bone loss.
The Consequences of Bone Loss After Tooth Extraction
It doesn't just affect the bone; it can impact the nearby tissues, oral health, and how your face looks.The gums of neighboring teeth may recede
Bone loss can spread to affect neighboring teeth lining the extracted tooth. As the bone shrinks, the surrounding gum tissue may recede, exposing the roots and causing the teeth to appear longer than usual.
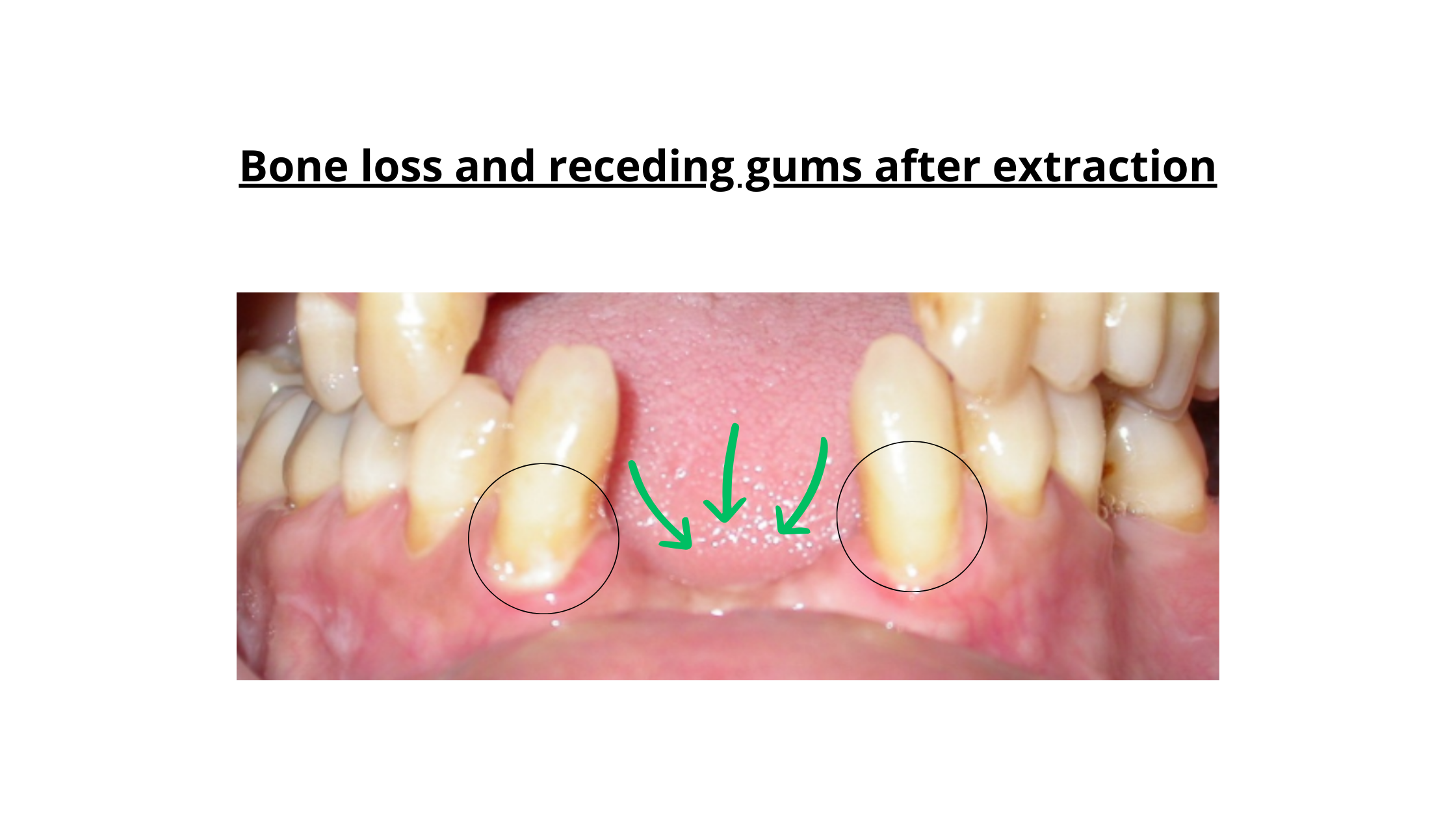
Beyond affecting the smile's appearance, receding gums can give rise to various dental issues, including tooth sensitivity and root decay.
Bone loss can be self-fuelling over time
After extraction, as the bone undergoes resorption, neighboring teeth start to shift to fill the space left by the missing tooth. The adjacent teeth move horizontally, while the opposing tooth shifts vertically.
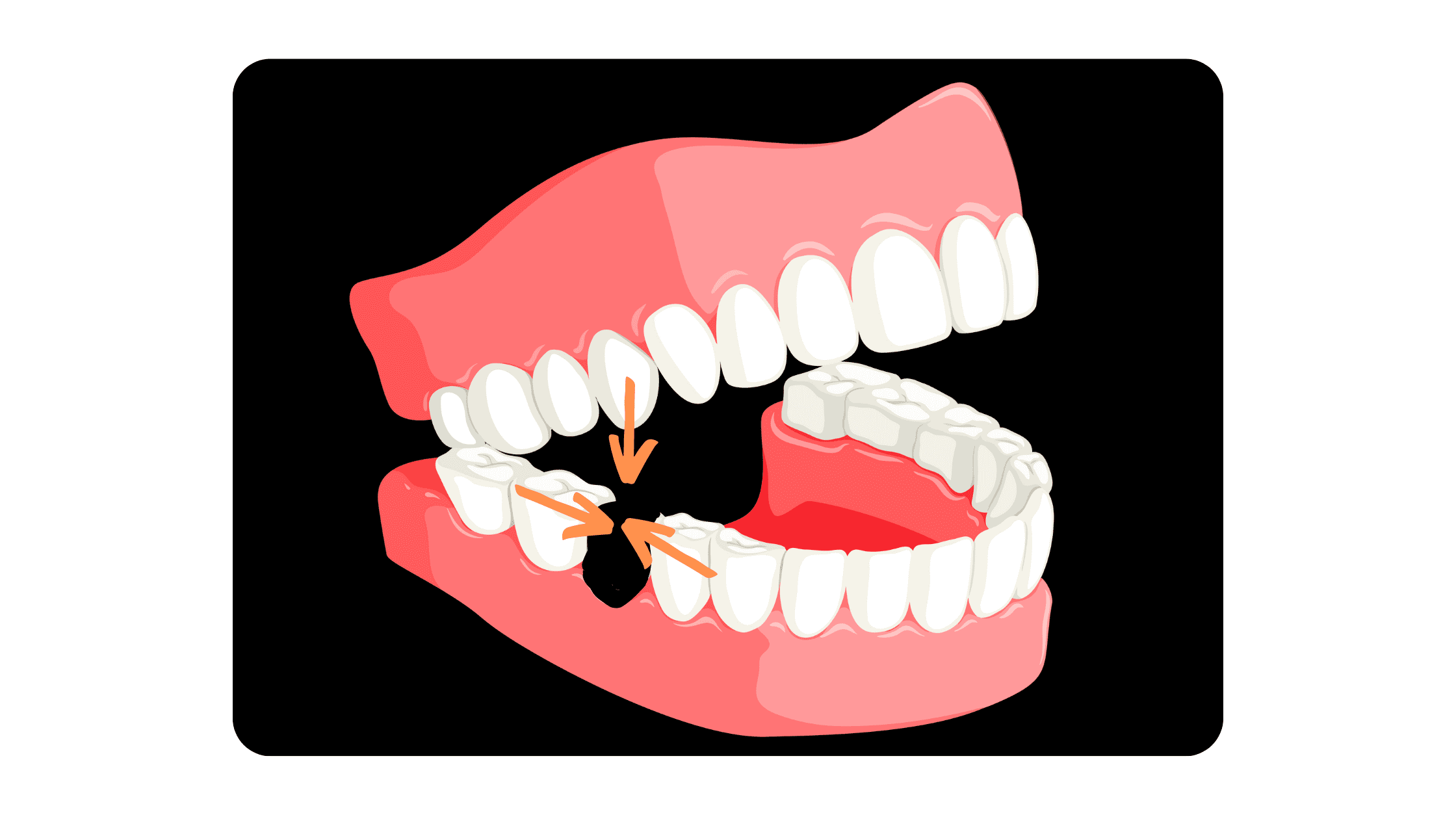
The opposite tooth in the other jaw will continue to move until it finds a contact point. As it migrates, it loses its bone and gum support, causing it to loosen and eventually fall out.
These natural dental shifts create gaps between the teeth, encouraging the accumulation of plaque and food. Some bacteria, known for their aggressiveness, can infiltrate the tissues and trigger inflammation. These reactions can erode and eat away at tissues, ultimately worsening bone loss.
Initially affecting the top portion of the bone supporting the teeth, resorption can extend to the underlying jawbone, resulting in various aesthetic and functional problems.
Your Face can sag and look older
The lower third of the face relies heavily on the support provided by the teeth and jaws.
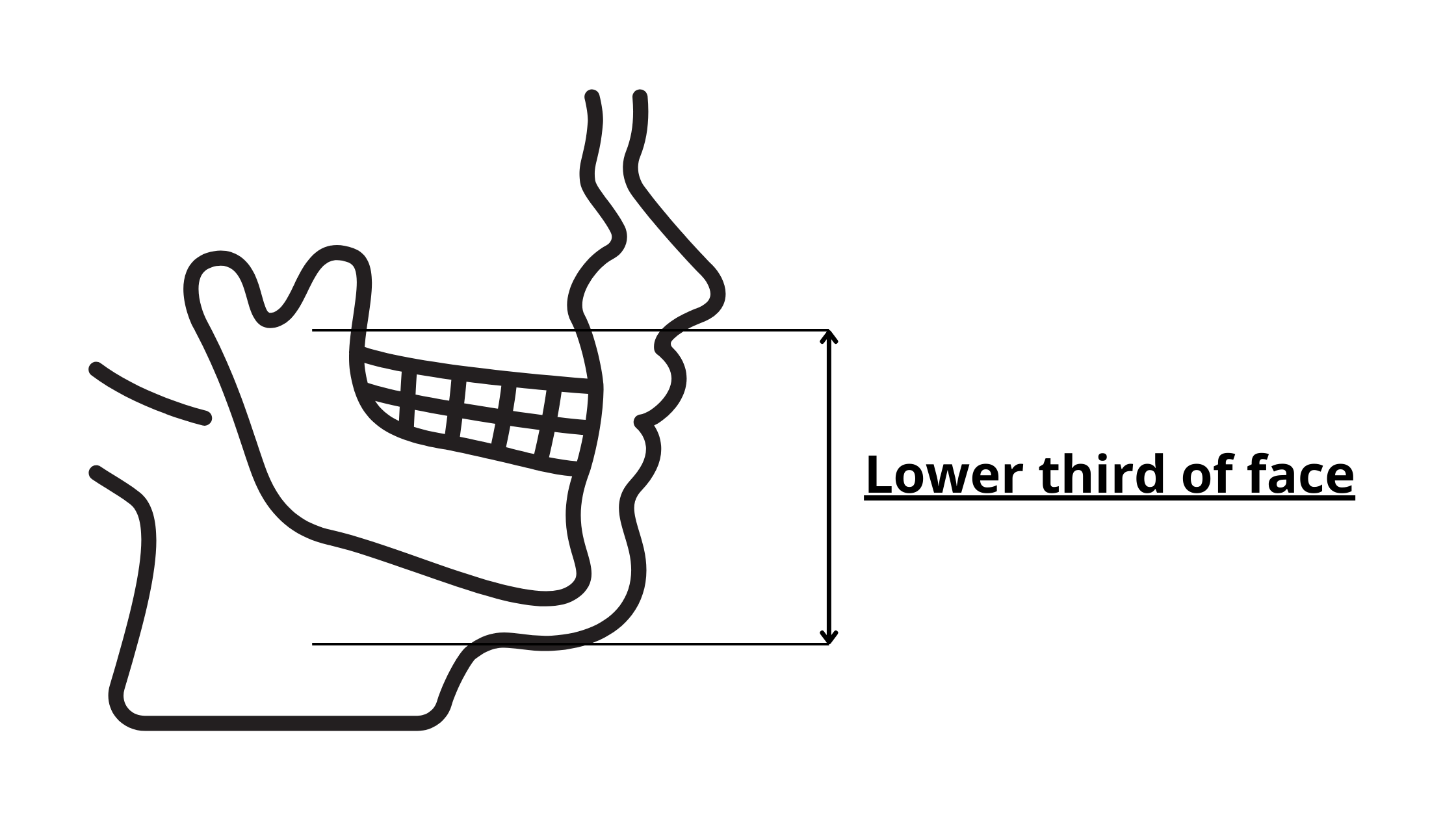
Tooth loss and subsequent jawbone loss can impact facial features, resulting in premature aging.
The collapse of the jawbone reduces the height of the lower face, bringing the chin closer to the nose and causing it to protrude forward.
With less support, the lips and cheeks lose elasticity, thin out, and sink into the mouth, accentuating wrinkles.
These changes not only affect facial attractiveness but also complicate teeth replacement treatments.
Additionally, a jaw that has lost significant bone is more prone to cracking or breaking with minimal impact.
Significant Bone Loss can Make Implant Placement challenging
For those considering dental implants to replace missing teeth, the height and thickness of the bone are crucial factors.
If a considerable amount of time has passed since tooth extraction, bone resorption could lead to a significant loss of jawbone volume.
Implant placement can become more challenging, though not impossible. There are now innovative techniques for restoring bone volume and adapting the size of implants to what is available.
Effects on Self-Confidence and Self-Esteem
In our appearance-focused society, tooth extraction and the subsequent changes can impact the facial and smile's aesthetics, making a person appear older than their actual age.
The impact on self-esteem and self-confidence can be significant. Some people may come to avoid social interaction for fear of revealing a smile they're unhappy with. This is particularly true for visible front teeth, such as incisors or canines, which can become a source of anxiety.
Fortunately, there are several options for preventing and treating bone loss. These options make it possible to successfully replace the missing tooth and regain an attractive, functional, and youthful smile.
Can Lost Bone Be Rebuilt?
You've undergone tooth extraction in the past and, due to a delay in replacement, significant bone loss has occurred. Now that you want to consider implants, a challenge arises – a specific volume of bone is necessary for this option.The good news is that multiple options exist to rebuild and strengthen the jawbone. The most suitable choice for you will depend on your unique situation. Here are some available options:
Guided Tissue Regeneration
In the complex wound healing process, it's like a race where different types of cells are competing to be the first to reach the wound and initiate tissue regeneration. Bone-forming cells, being a bit slower, might let other soft tissues take over the wound. This means the wound will heal with soft tissue, leaving no room for bone to form.
That's where guided tissue regeneration comes in. It creates a space above the jawbone, protected and isolated by a membrane. This helps bone cells take their time to build bone while stopping other cells from getting in the way.
Bone Block Grafting
This procedure involves placing a bone graft block onto the jawbone to strengthen it and restore its volume (both height and thickness).
There are two types of bone grafts: autogenic and allogenic.
Autogenic grafting uses bone from your own body, typically from the mouth or other areas like the skull or hip. Essentially, you become your own bone donor.
On the other hand, allogeneic grafting involves using bone from another person, with the bone undergoing thorough treatment before use.
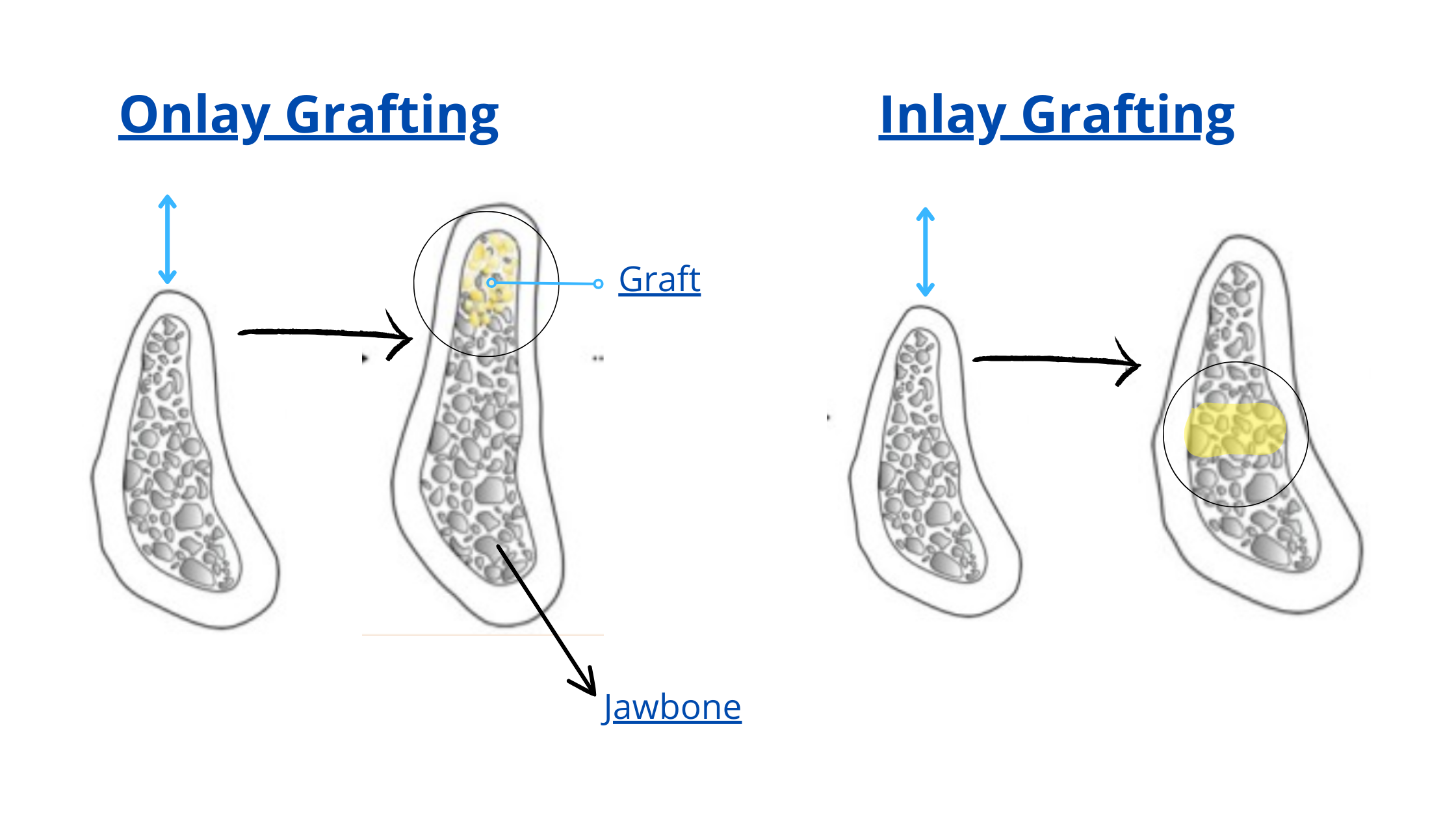
Bone block grafting can take two forms: onlay, where the bone is positioned on the external surface of the jawbone, or inlay, where the graft is placed between two bone segments.
Segmental Osteotomy
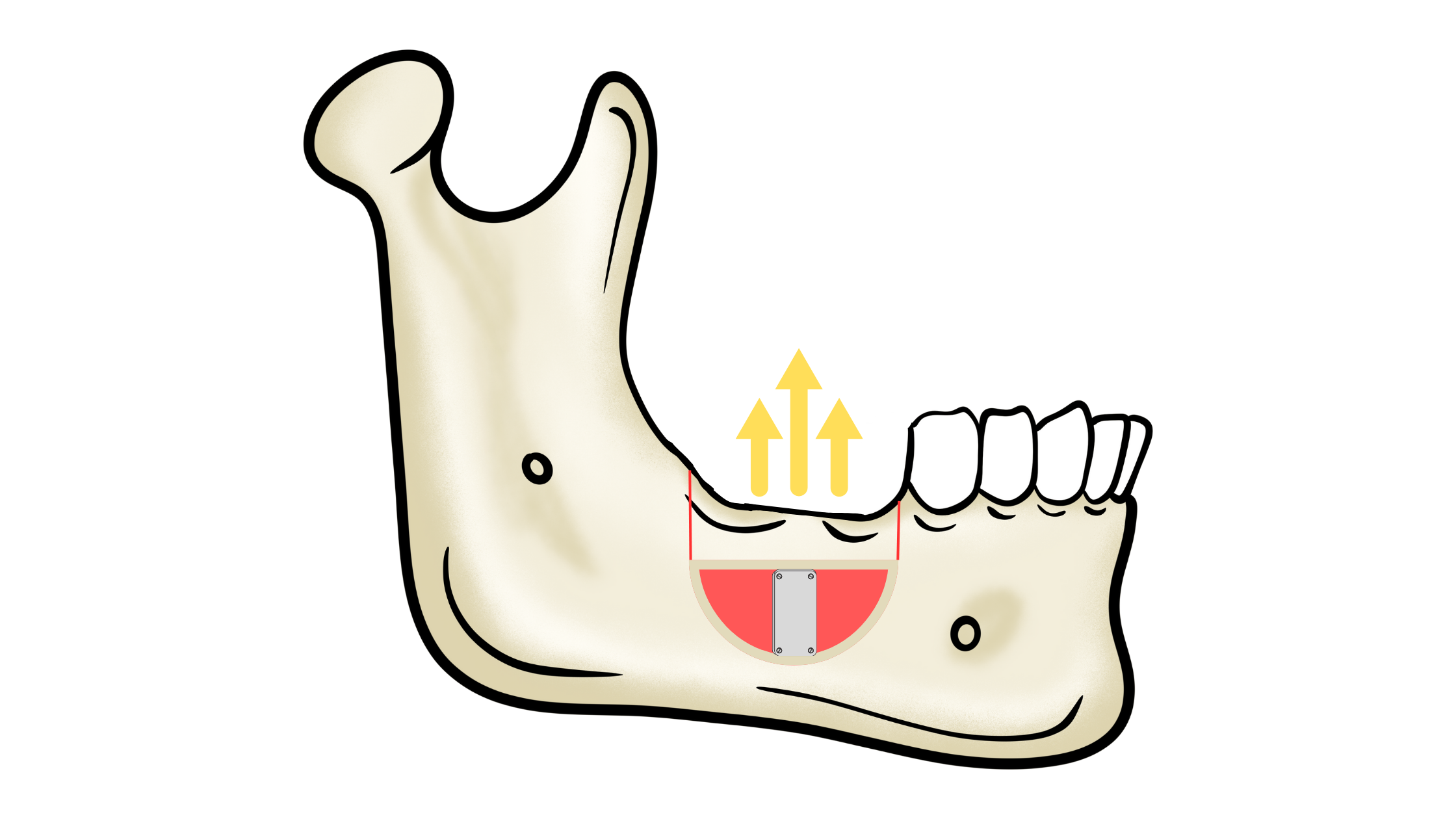 This technique is focused on raising the height of the jawbone. It consists of cutting a section of the bone, elevating it, and securing it in place. The gap left is then filled with graft material to promote healing.
This technique is focused on raising the height of the jawbone. It consists of cutting a section of the bone, elevating it, and securing it in place. The gap left is then filled with graft material to promote healing.
Sinus Lifting
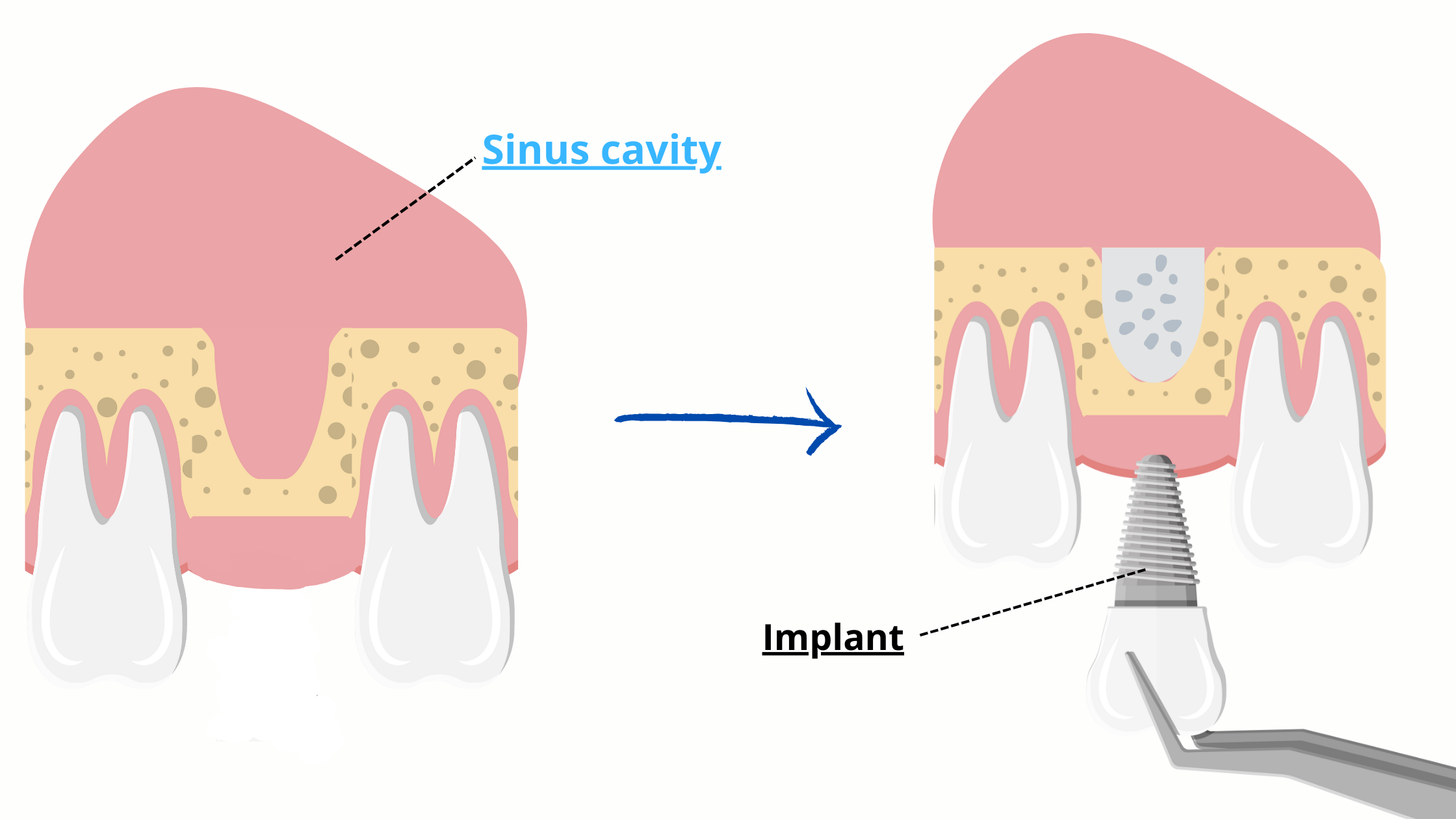
This technique is used specifically following the extraction of the back teeth in the upper jaw, located just beneath the sinuses.
The sinuses are air-filled cavities on each side of the cheeks. When an upper back tooth is removed, the sinus cavity above it can enlarge and shift downward, leading to a reduction in bone volume that cannot adequately support implants.
Sinus lifting addresses this issue by introducing a bone graft into the lower section of the sinuses. This process enhances the height of the available bone, preparing it for the implant that will be placed in the future as scheduled.
Prevent bone loss after extraction in the first place
The most effective approach to overcome bone loss after extraction is to prevent it from occurring in the first place. During and after the procedure, several steps can be taken, both by the dentist and you at home.The key thing to prevent post-extraction bone loss is to remember the primary culprit - the absence of stimulation from the teeth.
While there are various options for replacing missing teeth, dental implants stand out as the sole solution capable of preventing long-term bone loss. They are artificial roots that can mimic the natural role of teeth by stimulating the alveolar bone and maintaining its volume.
What Your Dentist Can Do:
- Gentle Tooth Extraction: Your dentist aims to extract the tooth with minimal trauma to avoid damaging the bone walls. The gentler the extraction technique, the less bone resorption will occur in the following months.
- Socket Preservation: This technique involves filling the empty socket with bone graft material immediately after tooth extraction. It significantly slows down and reduces bone resorption both vertically and horizontally. Your dentist may recommend this option, especially if you are more prone to bone loss due to factors like thin tissue biotype or pre-existing weak or damaged bone.
- Immediate Implant Placement: In this technique, the implant is placed during the same session as the tooth extraction. Bone grafting is applied to the implant site for stability and integration. Over time, the implant fuses with the surrounding jawbone, allowing for the placement of a crown.
A study noted a bone gain of 1.96 mm around immediately placed implants compared to those placed after healing.
While beneficial, this technique demands skill and may not be suitable for everyone. Factors like inadequate bone support or a thin tissue biotype might make socket preservation a more suitable option, providing time for tissue healing before considering an implant. - Planning implants in the future: In some cases, waiting for 4 to 6 months for the bone to mature before implant placement is preferable. However, this should not be delayed for too long, as bone loss is more pronounced in the initial year. Work closely with your dentist to determine the best timing based on your needs.
What you can do on your side
While some bone loss is natural and expected during the healing process after tooth extraction, you can slow it down and prevent it from worsening.
- Protect the Blood Clot (immediately after the procedure): Immediately after extraction, be careful not to disturb the blood clot that fills the socket. Dislodging it too soon can not only be painful, but can also cause bleeding, delay healing, and lead to more pronounced bone resorption.
- Maintain Oral Hygiene: Keep the extraction site inflammation-free by practicing good oral hygiene. Brush and clean between your teeth regularly to prevent the build-up of plaque and bacteria, which can contribute to further bone loss.
- Regular visits to the dentist: Regular dental check-ups for professional cleaning and thorough examinations help catch and treat oral conditions at their earliest stages.
- Ensure Nutrient Intake: Bone formation and maintenance rely on nutrients like calcium, phosphorus, and vitamins D, A, and C. Ensure you meet your daily requirements for these essential nutrients to strengthen your bones and enhance your overall health.
- Timely Tooth Replacement: Don't delay treatment to replace the missing tooth. Without proper stimulation, the bone may continue to shrink, making future treatment more challenging. Acting quickly is the key to optimal long-term results.
Sources
- Prevent the osseous resorption for a better integration of the complete removable prosthetic rehabilitations https://aos.edp-dentaire.fr/articles/aos/pdf/2016/07/aos2016280article2.pdf
- Effect of Alveolar Ridge Preservation after Tooth Extraction https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4293706/
- A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans http://dermatologiebuccale-nice.fr
